Heroes in Medical Research: The Postdoctoral Fellow
Writer: Stephen J. Williams, Ph.D
The National Postdoctoral Association (NPA) had its Fifth Annual Celebration Of National Postdoc Appreciation Week (NPAW) in September and I wanted to focus a posting on curating stories from postdoctoral fellows as well as private investigators (PIs) and mentors on the impacts that postdoctoral fellows had in research and to recognize the critical and tremendous contributions which postdocs make to science.
During our postdoctoral years, we develop deep friendships which last a lifetime, a close bonding to our kindred scientists different in nature than our bonding with our mentors. Nothing can replace a great mentor but our fellow postdocs make a huge difference in our complete scientific training.
It’s always the little things that stand out in our fondest memories
Unfortunately I have a plethora of fond, little memories; too many for this posting but just want to ad in a few things:
- Thank you! – To all those postdocs who worked tirelessly to make a memorable PostDoc Day!
- Thank you! – To all my postdoc colleagues who stayed late n the lab with me giving each other moral and scientific support
- Thank you! – All my postdoc friends who would give up their time to show me how to make and use a text box correctly in Word
- Thank you! =- for your friendship and understanding in those rough times we had experienced
To enliven the discussion, I ask that postdocs, past, present, and future, as well as PI’s and postdoc mentors comment on their postdoc experience. I also would like PI’s to share the stories how their postdocs made an impact to their labs.
A few interesting links and articles from the web on the importance and struggles of postdocs are included below:
Keith Micoli, from New York University Langone Medical Center states in an Elsevier article on The Academic Executive Brief
“
Consequently, it’s very difficult to come up with accurate numbers. Current estimates on number of postdocs come between 40,000 and 90,000 — a range that is unacceptable. A solid bet is that there are 60,000 postdocs and that more than half, if not two thirds or higher, are international.
– from US research enterprise powered by international postdocs by Keith Micoli at NYU
“
Survey Methodology
Since Science started conducting annual surveys seven years ago, alternating between polling postdocs and postdoc advisors, the attributes that survey respondents select as being most important to a successful postdoc have not varied much.This year’s survey was launched on March 15, 2011, with e-mail invitations sent out to about 40,000 current and former postdoc advisors worldwide. Of the 798 completed surveys that were collected, 71 percent came from Europe (39 percent) and North America (32 percent). The remaining respondents were located in Asia/Australia/Pacific Rim (20 percent) or other areas of the world (9 percent). Most were males (72 percent) 40 years of age and older (76 percent) and worked in academic institutions (70 percent) and government organizations (13 percent). The primary area represented was the life sciences (57 percent).
However only a handful of institutions were featured.
An open letter to AAAS journal “Science”: Postdocs need to address the “The Future of Research”
- Gary McDowell 1
- Kristin Krukenberg 2
- Jessica Polka 2
This letter, posted on the Winnower.com, was a response to Callier’s article “Ailing academia needs culture change”1 and discussed how postdoctoral fellows have to lead in effecting change if the US research enterprise is to flourish in the future. In addition, the authors have been organizing Boston area postdoctoral associations and are sponsoring a symposium to be held at Boston University October 2-3 2014, focusing on the challenges facing graduate students and postdoctoral fellows: the “Future of Research” symposium (futureofresearch.org, @FORsymp).
- V. Callier, N. L. Vanderford. “Ailing academia needs culture change.” Science, 2014: 345; 6199: 885. DOI: 10.1126/science.345.6199.885-b
On the surface, many acknowledge the importance of postdoctoral fellows to the US research effort,
HOWEVER, the QUESTION remains DO POSTDOCS FEEL APPRECIATED FOR THEIR EFFORTS?
Please read Jacquelyn Gil, Ph.D.’s GREAT blog post
Have you hugged your postdoc today?
in The Contemplative Mammoth about her surviving postdoctoral life.
For some postdoc humor go to
http://phdcomics.com/comics.php where Jorge Cham, Ph.D. has been satiring the Ph.D. life since he was a graduate student in the late 90’s.
and see if you could be a star in their movie about Ph.D.’s: The PhD Movie and the sequel.
Don’t Underestimate Your Postdoc
Dr. Thomas C. Sudhof, MD is an example of a postdoctoral fellow making great contributions to a lab. A summary of his work is seen below and obtained from the site thebestschools.org on the “50 Most Influential Scientists”.
http://www.thebestschools.org/features/50-influential-scientists-world-today/#S%C3%BCdhof
Thomas C. Südhof
Thomas C. Südhof is a biochemist and professor in the School of Medicine in the Department of Molecular and Cellular Physiology at Stanford University. He is best known for his work in the area of synaptic transmission, which is the process by which signaling chemicals known as neurotransmitters are released by one neuron and bind to and activate the receptors of another neuron.
Südhof won the 1985 Nobel Prize in Physiology or Medicine, along with Randy Schekman and James Rothman.
Südhof, a native of Germany, obtained his MD from the University of Göttingen and conducted his postdoctoral training in the department of molecular genetics at the University of Texas’s Health Science Center. During his postdoctoral training, he worked on describing the role of the LDL receptor in cholesterol metabolism, for which Michael S. Brown and Joseph L. Goldstein were awarded the Nobel Prize in Physiology or Medicine in 1985.
Another example from the site includes Dr. Craig Mello (Craig C. Mello’s Home Page.) who, along with Dr., Andrew Fire discovered RNAi when both at Carnegie Institute. Both received a Nobel for their work.
So again would love to hear and curate personal stories highlighting how postdocs make a great contribution to US science.
More articles in this “Heroes in Medical Research” series and posts on Scientific Careers from this site include:




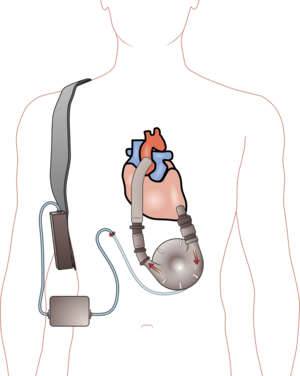

 The American Heart Association presented its prestigious Paul Dudley White Award to
The American Heart Association presented its prestigious Paul Dudley White Award to