Proteins that control neurotransmitter release
Author & Curator: Larry H. Bernstein, MD, FCAP
Richard H. Scheller, PhD

The sec6/8 Complex Is Located at Neurite Outgrowth and Axonal Synapse-Assembly Domains
Christopher D. Hazuka, Davide L. Foletti, Shu-Chan Hsu, Yun Kee, F. Woodward Hopf, and Richard H. Scheller
Department of Molecular and Cellular Physiology, Howard Hughes Medical Institute, Stanford University School of Medicine, Stanford, California 94305-5428
The Journal of Neuroscience, February 15, 1999, 19(4):1324–1334 http://www.jneurosci.org/content/19/4/1324.full.pdf
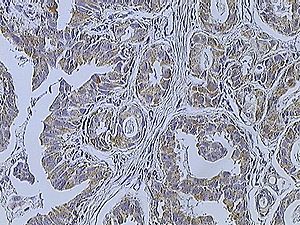
The molecules that specify domains on the neuronal plasma membrane for the delivery and accumulation of vesicles during neurite outgrowth and synapse formation are unknown. We investigated the role of the sec6/8 complex, a set of proteins that specifies vesicle targeting sites in yeast and epithelial cells, in neuronal membrane trafficking. This complex was found in layers of developing rat brain undergoing synaptogenesis. In cultured hippocampal neurons, the sec6/8 complex was present in regions of ongoing membrane addition: the tips of growing neurites, filopodia, and growth cones. In young axons, the sec6/8 complex was also confined to periodic domains of the plasma membrane. The distribution of synaptotagmin, synapsin1, sec6, and FM1–43 labeling in cultured neurons suggested that the plasma membrane localization of the sec6/8 complex preceded the arrival of synaptic markers and was downregulated in mature synapses. We propose that the sec6/8 complex specifies sites for targeting vesicles at domains of neurite outgrowth and potential active zones during synaptogenesis. Key words: synaptogenesis; neurotransmission; secretion; exocytosis; synaptic vesicle; vesicle targeting
Targeting of vesicles to synaptic sites during development may use similar mechanisms as those involved in vesicle fusion underlying membrane outgrowth. Before contact with a postsynaptic target, axons possess mobile vesicle clusters bearing synaptotagmin, which fuse with the plasma membrane after stimulation (Matteoli et al., 1992; Kraszewski et al., 1995; Dai and Peng, 1996). Thus, growing axons must contain the molecular machinery required for constitutive exocytosis, endocytosis, and activitydependent vesicle release. However, it is unclear how vesicles become clustered at synapses. Although vesicle fusion in axons might occur anywhere along the plasma membrane, there must be membrane targets that signal the clustering of vesicles for synapse formation. Furthermore, it is unclear how sites of vesicle exocytosis are modified as the neuron forms stable contacts with postsynaptic partners.
Identification of a Novel Rab11/25 Binding Domain Present in Eferin and Rip Proteins
Rytis Prekeris*, Jason M. Davies*, and Richard H. Scheller#
JBC Papers in Press. Published on July 31, 2001 as Manuscript M106133200
http://www.jbc.org/content/early/2001/07/31/jbc.M106133200.full.pdf
Rab11, a low molecular weight GTP binding protein, has been shown to play a key role in a variety of cellular processes, including endosomal recycling, phagocytosis, and transport of secretory proteins from the TGN. In this study we describe a novel Rab11 effector, EF hands containing Rab11 interacting protein (eferin). In addition, we identify a 20 amino acid domain that is present at the C-terminus of eferin and other Rab11/25 interacting proteins, such as Rip11 and nRip11. Using biochemical techniques we demonstrate that this domain is necessary and sufficient for Rab11 binding in vitro and that it is required for localization of Rab11 effector proteins in vivo. The data suggest that various Rab effectors compete with each other for the binding to Rab11/25 possibly accounting for the diversity of Rab11 functions.
Members of the Rab/Ypt GTPase family have emerged as important regulators of vesicular trafficking (1). Rab proteins have been proposed to mediate a variety of functions, including vesicle translocation and docking at a specific fusion sites. Like all small GTPases, Rabs cycle between active (GTP bound) and inactive (GDP bound) conformations (2). In the GTP bound state, Rab proteins can bind a variety of downstream effector proteins, while GTP hydrolysis leads to a conformational change in the “switch” region that renders the Rab GTPase unrecognizable to its effector proteins (3,4). A key question in understanding the interactions between Rabs and their effectors concerns the mechanisms by which Rab GTPases specifically bind a diverse spectrum of effectors and how this is regulated by the common structural motif used as a GTP switch. Biochemical and genetic studies have identified several hypervariable regions that might be involved in determining Rab specificity, including N- and C-termini, as well as α3/β5 by guest on September 6, 2015 http://www.jbc.org/ Downloaded from loop (5,6). Indeed, the recently reported structure of Rab3a bound to a putative effector, rabphillin-3a, revealed that Rab3a/rabphillin-3a complex interacts through two main regions (7). The first consists of conformationally sensitive “switch” regions of Rab3a bound to the a1 helix and the C-terminal part of rabphillin-3a. The second involves the SGAWFF domain of rabphillin-3a which fits into a pocket formed by the three hypervariable complementary determining regions (CDRs) of Rab3a, corresponding to the N- and C-termini and α3/β5 loop. Thus, it appears that the hypervariable RabCDR are involved in determining the specificity of effector binding, while the conserved “switch” regions impart GTP dependency and binding. It remains to be determined, however, whether this paradigm also applies to other Rab/effector complexes. Rab11a, -11b, and -25 are closely related members of Rab GTPase family that have been implicated in regulating a variety of different post-Golgi trafficking pathways, such as protein recycling (8), phagocytosis (9), insulin-stimulated Glut4 insertion in the plasma membrane (10), and membrane trafficking from early endosomes to the transGolgi network (11). During the last few years several Rab11/25 interacting proteins have been identified, including Rab11BP/Rabphilin-11, Rip11, nRip11, and myosin Vb (12- 15). However, the mechanisms of their function, as well as molecular aspects of their interactions with Rab11, remain to be fully understood. In the present study, we report the identification of EF-hands containing Rab11/25 interacting protein (eferin). Furthermore, we characterized a Rab binding domain (RBD11) which is present at the Cterminus of eferin as well as other Rab11/25 binding proteins, such as Rip11 and nRip11. Using biochemical techniques we demonstrated that RBD11 is the region which encodes the specificity for Rab11/25, but is distinct from the region interacting with Rab “switch” domain, since its interactions with the Rab11/25 are not GTP-dependent.
The functional significance of the differences in Rip and eferin interactions with Rab11/25 remains to be determined. One possibility is that additional cellular factors can regulate the affinity of Rab11/25 binding to its effectors. Indeed, the recombinant full length Rip11 binds poorly to Rab11a in pull down and yeast-two hybrid assays as compared to full length endogenous Rip11 from cellular TX-100 extracts (data not shown). Furthermore, it has been previously shown that Rip11 can also interact with γSNAP and cytoskeleton (13,24). Thus, the interactions of Rips and eferin with different factors could be used as a means of differentially regulating Rab11/25 binding. Alternatively, the Rab11/25 binding motif in eferin and Rip11 might be conformationlly hidden and require activation before binding to Rab11/25. We have previously demonstrated that phosphorylation of Rip11 plays an important role in its trafficking (13). Thus, differential phosphorylation on Rab11/25 binding motifs could also play a role in regulating the binding of Rip11 and eferin to Rab GTPases. Despite to recent progress in understanding the roles of Rabs and their effectors in regulating membrane trafficking, we are only beginning to unravel the structural determinants of their function. Identification and characterization of the Rab11/25 binding regions in Rip and Eferin proteins will be of a crucial importance in understanding the molecular mechanisms involved in differential regulation of the variety of Rab11-dependent trafficking pathways.
Richard H Scheller, PhD
The Keck School of Medicine of USC is the first medical school in the nation to host the Lasker Lectures, featuring recipients of the prestigious 2013 Albert Lasker Basic Medical Research Award. In this installment, Richard H. Scheller, PhD, executive vice president of Genentech research and early development, discusses breakthoughs in drug development that are turning the tide in the war against cancer.
Kavli Prize 2015
Xenon Pharmaceuticals Appoints Dr. Richard H. Scheller to Its Board of Directors http://fb.me/78z2HoJKa
Biopharmaceutical company Xenon Pharmaceuticals (NasdaqGM:XENE) reported on Monday the addition of Richard H. Scheller, PhD to its board of directors.
Most recently, Dr Scheller has served as chief science officer and head of Therapeutics at 23andMe.
Previously Dr Scheller was the executive vice president at Genentech Research and Early Development & a member of the Roche Corporate Executive Committee; chief scientific officer, executive vice president of Research and senior vice president of Research at Genentech; as well as a professor of Molecular and Cellular Physiology and of Biological Sciences at Stanford University Medical Center and an investigator of the Howard Hughes Medical Institute.
Dr Scheller is currently an adjunct professor in the Department of Biochemistry and Biophysics, School of Medicine at the University of California, San Francisco.
He has been a Director at Xenon Pharmaceuticals Inc. since March 16, 2015 and Medrio, Inc. since November 2012. He serves as a Member of the Medical and Scientific Review Board of Evotec (US), Inc. (Renovis Inc.). In 2014, he was named a trustee of Caltech. He served as a Member of Scientific Advisory Board of Intra-Cellular Therapies, Inc. and Rinat Neuroscience Corporation.
He served on numerous advisory boards including the National Advisory Mental Health Council of the National Institutes of Health. Dr. Scheller served as chairman of the Genentech Foundation’s board of directors. He is a globally recognized leader in biomedical research.
He has published over 200 papers in scientific journals, and worked in cell biology. He has received several additional awards for his work elucidating the molecular mechanisms governing neurotransmitter release, including the 2013 Albert Lasker Basic Medical Research Award, the 2014 California Institute of Technology’s Caltech Distinguished Alumni Award, the 2010 Kavli Prize in Neuroscience, and the 1997 U.S. National Academy of Sciences Award in Molecular Biology. He is a Fellow of the American Academy of Arts and Sciences. Dr. Scheller holds a Doctorate in Chemistry from the California Institute of Technology in 1980, where he was also a Postdoctoral Fellow, Division of Biology. He was also a Postdoctoral Fellow at Columbia University, College of Physicians & Surgeons. He has Bachelor’s Degree in Biochemistry in 1975 at the University of Wisconsin, Madison.
Education: 1971-1975 University of Wisconsin-Madison B.S. – Biochemistry with Honors 1975-1980 California Institute of Technology Ph.D. – Chemistry – Advisor: Eric H. Davidson 1980-1981 California Institute of Technology Postdoctoral Fellow-Division of Biology Advisor: Eric H. Davidson 1981-1982 Columbia University-College of Physicians & Surgeons Postdoctoral Fellow-Molecular Neurobiology Advisors: Richard Axel and Eric R. Kandel Industry Positions: 2001-2003 Senior Vice President – Research Genentech, Inc. 2003-2009 Executive Vice President – Research Genentech, Inc. 2008-2009 Chief Scientific Officer and Executive Vice President – Research Genentech, Inc. 2009- Executive Vice President – Genentech Research and Early Development (gRED) and Member of the Enlarged Roche Corporate Executive Committee Academic Appointments: 1982-1987 Assistant Professor, Department of Biological Sciences, Stanford University 1987-1990 Associate Professor, Department of Biological Sciences, Stanford University 1990-1993 Associate Professor, Department of Molecular and Cellular Physiology, Stanford University Associate Professor (by courtesy), Department of Biological Sciences, Stanford University