Contributions to the Study of the Etiology of a Cardiovascular Disorder:
Congenital Heart Disease (CHD) at Birth and into Adulthood: The Role of Spontaneous Mutations
Curator: Aviva Lev-Ari, PhD, RN
THE ETIOLOGY OF Congenital Heart Disease (CHD)
Congenital heart disease is a problem with the heart’s structure and function that is present at birth.
Causes
Congenital heart disease (CHD) can describe a number of different problems affecting the heart. It is the most common type of birth defect. Congenital heart disease causes more deaths in the first year of life than any other birth defects.
Congenital heart disease is often divided into two types: cyanotic (blue skin color caused by a lack of oxygen) and non-cyanotic. The following lists cover the most common congenital heart diseases:
Cyanotic:
- Ebstein’s anomaly
- Hypoplastic left heart
- Pulmonary atresia
- Tetralogy of Fallot
- Total anomalous pulmonary venous return
- Transposition of the great vessels
- Tricuspid atresia
- Truncus arteriosus
Non-cyanotic:
- Aortic stenosis
- Atrial septal defect (ASD)
- Atrioventricular canal (endocardial cushion defect)
- Coarctation of the aorta
- Patent ductus arteriosus (PDA)
- Pulmonic stenosis
- Ventricular septal defect (VSD)
These problems may occur alone or together. Most children with congenital heart disease do not have other types of birth defects. However, heart defects can be part of genetic and chromosome syndromes. Some of these syndromes may be passed down through families.
Examples include:
- DiGeorge syndrome
- Down syndrome
- Marfan syndrome
- Noonan syndrome
- Trisomy 13
- Turner syndrome
Often, no cause for the heart disease can be found. Congenital heart diseases continue to be investigated and researched. Drugs such as retinoic acid for acne, chemicals, alcohol, and infections (such as rubella) during pregnancy can contribute to some congenital heart problems.
Poorly controlled blood sugar in women who have diabetes during pregnancy has also been linked to a high rate of congenital heart defects.
Symptoms
Symptoms depend on the condition. Although congenital heart disease is present at birth, the symptoms may not appear right away.
Defects such as coarctation of the aorta may not cause problems for many years. Other problems, such as a small ventricular septal defect (VSD), may never cause any problems. Some people with a VSD have a normal activity level and lifespan.
Exams and Tests
Most congenital heart defects are found during a pregnancy ultrasound. When a defect is found, a pediatric heart doctor, surgeon, and other specialists can be there when the baby is delivered. Having medical care ready at the delivery can mean the difference between life and death for some babies.
Which tests are done on the baby depend on the defect, and the symptoms.
Treatment
Which treatment is used, and how well the baby responds to it, depends on the condition. Many defects need to be followed carefully. Some will heal over time, while others will need to be treated.
Some congenital heart diseases can be treated with medication alone. Others need to be treated with one or more heart surgeries.
Prevention
Women who are expecting should get good prenatal care:
- Avoid alcohol and illegal drugs during pregnancy.
- Tell your doctor that you are pregnant before taking any new medicines.
- Have a blood test early in your pregnancy to see if you are immune to rubella. If you are not immune, avoid any possible exposure to rubella and get vaccinated right after delivery.
- Pregnant women who have diabetes should try to get good control over their blood sugar levels.
Certain genes may play a role in congenital heart disease. Many family members may be affected. Talk to your health care provider about genetic screening if you have a family history of congenital heart disease.
The Role of Spontaneous Mutations – The Genes and The Pathways:
Contributing Researchers’ Bio
| HHMI INVESTIGATOR 1994– Present Yale School of Medicine |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Richard P. Lifton, M.D., Ph.D. |

Twenty years ago, when Richard Lifton first proposed using genetic methods to study the causes of high blood pressure, his approach was not uniformly accepted. Such a complicated condition, critics thought, would not lend itself to traditional genetic tactics, which try to link a disease to alterations in a single gene. Since then, Lifton has proved his detractors wrong many times over. Lifton has identified more than 20 genes associated with blood pressure, cardiovascular disease, and bone density, and he has characterized mutations that cause either extreme hypertension (high blood pressure) or hypotension (low blood pressure) in people. More significantly, he has shown that severe blood pressure problems can be caused by mutations in genes that regulate the amount of sodium chloride the kidney allows to flow into the blood. When these genes falter in severe hypertension cases, salt levels rise, blood volume increases, the heart pumps harder, and blood pressure surges. With excessive hypotension, the opposite occurs. Today, his findings have changed how doctors treat hypertension, which affects approximately 1 billion people worldwide and is the most prevalent cardiovascular disease risk factor. At the time Lifton started looking for blood pressure genes, scientists and clinicians did not know if the brain, cardiovascular system, adrenal gland, or kidney was the primary source of the problem. Cardiologists tended to consider the heart or the vascular system as the blood pressure regulator. Others thought the adrenal gland hormone aldosterone, which regulates blood salt and potassium levels, was the master controller. To better understand hypertension’s pathophysiology, Lifton borrowed the concept behind classic fruit fly genetics and applied it to humans. Scientists would treat insects with mutagens and see dramatic effects in progeny wing shape or eye color and then find the gene that caused the altered trait. Since mutagenesis experiments cannot be performed in humans, Lifton instead sought the most extreme cases of severe blood pressure disease. A person with hypertension needing treatment has blood pressure readings above 140/90. But Lifton was interested in rare individuals with both very high and low measurements. Physicians and scientists throughout the world have contacted him. “Today, people even find me on the Internet,” he says. Lifton studies the families, determines inheritance patterns, takes blood samples, and ultimately localizes genes and mutations responsible for their conditions. He estimates he has collected blood samples from more than 10,000 people. “I always have been struck by how willing people are to participate in research when a disease runs in their families,” Lifton said. “They know how the disease impacts their family and hope research might lead to benefits to future generations in their family and in others, too.” In 1994, Lifton first showed that a mutation in the kidney (in a sodium channel) could cause severe hypertension. “It was the first paper to demonstrate a mutation intrinsic to the kidney was critical for blood pressure homeostasis,” Lifton said. Since then, he has found mutations in 10 kidney genes that raise blood pressure and mutations in 9 kidney genes that lower blood pressure. All the mutations affect how the kidney regulates salt levels in the blood. Collectively, his work provided the scientific underpinnings for new national hypertension treatment guidelines. They recommend that most patients with hypertension take drugs called diuretics, which lower blood pressure by reducing kidney salt reabsorption. Reabsorption is when the kidney returns salt, glucose, and other plasma components back into the bloodstream after it has removed substances it will excrete in the urine. “Before these recommendations, hypertension treatment used to be completely empiric,” Lifton said, with doctors choosing among 70 different drugs that acted on the heart, blood vessels, or elsewhere, and seeing what worked for individual patients. His research also revealed the reason for a major side effect of diuretics, which is that patients crave and inadvertently consume excess salt, defeating the drug’s purpose. Such patients now are given another drug that represses their desire to eat salt. Although hypertension treatment has improved in the past two decades, less than a third of patients have their blood pressure adequately controlled because drugs do not work. As a result, they are more likely to have a heart attack or stroke. To bring better antihypertensive drugs to market, Lifton uses his knowledge about the kidney gene pathway and other novel cardiovascular disease genes he has discovered and collaborates with pharmaceutical industry scientists. Meanwhile, utilizing the new tools of genomics, which analyze many genes simultaneously, Lifton is searching for variations in the genes he first identified in rare cases to determine their possible contributions to blood pressure problems in the general population. Such research could lead to individualized treatment based on a genetic profile. With these new technologies, it may also be possible to prevent hypertension before damage occurs. Lifton pursued medicine and research because he was inspired as a boy by President John Kennedy’s call to public service. “Working with patients to understand human disease,” he said “and advancing knowledge and treatment is an enterprise of infinite fascination and reward.” Dr. Lifton is also Sterling Professor of Genetics and Internal Medicine at Yale School of Medicine.
Photo: Gayle Zucker |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Though no one in her family was a physician, Christine Seidman always wanted to be a doctor. But the word had a slightly different meaning for her than it does for most. “To me, that was a person who was medically trained and took care of sick people, but who also really understood why they got sick…Some people think you’re a physician or a scientist. To me, they’re synonymous. I still think that.”
Seidman—who goes by Kricket (thanks to a young cousin who couldn’t pronounce “Christine”)—met her husband and research partner, Jon, when they were both undergraduates at Harvard. “We had a lab research project that we had to design and have approved. My group’s project was not approved. So they split up our group and reassigned us to other projects, and I got assigned to Jon’s group.”
The two were married during Seidman’s junior year. After graduation and medical school, Seidman headed to Johns Hopkins for her residency and internship “because it spoke science to me.” She was there for three years before moving to Boston, where she did a cardiology fellowship at Massachusetts General Hospital before finishing her training in Baltimore.
At MGH, Seidman worked with a group led by the late Edgar Haber, trying to isolate and clone the genes for adrenergic receptors, which are important in cardiovascular physiology. She then became interested in atrial natriuretic peptide, or ANP. Released by the heart, ANP regulates salt and water in the bloodstream to reduce blood pressure. A partial amino acid sequence of this natriuretic peptide had just been published, and Seidman was intrigued; studying ANP had broad implications for treatment of high blood pressure. “As a cardiologist, you think this might cure hypertension.”
She moved to her husband’s lab at Harvard Medical School, where she cloned the ANP cDNA and gene. The two have worked together ever since, studying the effects of genetic variation in heart disease.
In 1998, she began studying disorders of heart muscle. Seidman’s work began with familial hypertrophic cardiomyopathy (HCM), which increases heart thickness and predisposes to the development of heart failure and sudden death. HCM is the most common cause of sudden death on the athletic field; it also affects many more people than originally thought. Seidman used genetic approaches to discover mutations that altered proteins involved in heart muscle contraction. This work enabled the development of models that can help researchers understand the mechanisms by which mutations cause disease. The work also allowed for gene-based diagnosis of HCM.
Seidman’s group also has identified gene mutations that cause dilated cardiomyopathy and congenital heart malformations.
To understand how gene mutations affect heart structure and function, Seidman’s laboratory does much of their work in mouse models. “If you know that a gene abnormality causes disease, you ought to be able to stick that gene into a cell and figure out the pathways it affects and what it does. But we don’t have any cell lines in cardiology. So we put the genes into mice and let them get heart disease and then study the heart.”
Most recently, Seidman used mice genetically destined for heart disease and a gene-sequencing technique called PMAGE to identify hundreds of early-acting genes that could be responsible for hypertrophic cardiomyopathy. This type of work could help scientists define the pathways that lead to cellular changes in this disease and other cardiac diseases, as well as identify targets for potential drug therapies.
“PMAGE represents an approach for mechanistic understanding of cardiac disease,” she says. “It’s a really in-depth way to look for genes that change early and cause responses that ultimately equal disease. We ought to be able to learn from these changes and perhaps alter them, so as to prevent or diminish the subsequent development of disease. While today this approach makes use of animal models, it will be equally powerful when applied to study diseased heart tissues from patients.”
The Seidmans have three children—14-year-old Gregor; 21-year-old Seth, a history major at Brown; and 25-year-old Nika, a medical student at Harvard. They live in Milton, Massachusetts, which Seidman likes because of its relatively rural flavor.
Outside the lab, “I am into heavy-duty gardening,” she says. “It’s more like landscape architecture. I think in my next life, I’ll be a botanist.”
Dr. Seidman is also Professor of Genetics and Medicine at Harvard Medical School and Director of the Cardiovascular Genetics Center at Brigham and Women’s Hospital, Boston.
![]()
RESEARCH ABSTRACT SUMMARY:
Christine Seidman is interested in understanding the genetic basis of human cardiovascular disorders such as cardiomyopathy (hypertrophic and dilated), heart failure, and congenital heart malformations. Using experimental models that are engineered to carry human mutations, her lab examines the consequences of mutations on cardiac biology that lead to clinical manifestations of disease. She hopes to combine knowledge of genetic etiologies and molecular mechanisms to improve therapeutic opportunities for patients.
View Research Abstract![]() Photo: Justin Knight
Photo: Justin Knight
MAY 12, 2013 Spontaneous Mutations Play a Key Role in Congenital Heart Disease Every year, thousands of babies are born with severely malformed hearts, disorders known collectively as congenital heart disease. Many of these defects can be repaired though surgery, but researchers don’t understand what causes them or how to prevent them. New research shows that about 10 percent of these defects are caused by genetic mutations that are absent in the parents of affected children. Although genetic factors contribute to congenital heart disease, many children born with heart defects have healthy parents and siblings, suggesting that new mutations that arise spontaneously—known as de novomutations—might contribute to the disease. “Until recently, we simply didn’t have the technology to test for this possibility,” says Howard Hughes Medical Institute (HHMI) investigator~Richard Lifton. Lifton, who is at Yale School of Medicine, together with Christine Seidman, an HHMI investigator at Brigham and Women’s Hospital and colleagues at Columbia, Mt. Sinai, and the University of Pennsylvania, collaborated to study congenital heart disease through the National Heart Lung and Blood Institute’s Pediatric Cardiac Genomics Consortium.
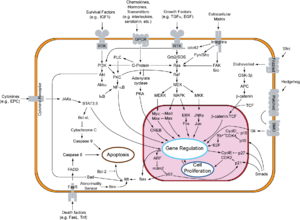
Using robust sequencing technologies developed in recent years, the researchers compared the protein-coding regions of the genomes of children with and without congenital heart disease and their parents, and found that new mutations could explain about 10 percent of severe cases. The results demonstrated that mutations in several hundred different genes contribute to this trait in different patients, but were concentrated in a pathway that regulates key developmental genes. These genes affect the epigenome, a system of chemical tags that modifies gene expression. The findings were published online in the journal Nature on May 12, 2013. For the current study, the investigators began with 362 families consisting of two healthy parents with no family history of heart problems and a child with severe congenital heart disease. By comparing genomes within families, they could pinpoint mutations that were present in each child’s DNA, but not in his or her parents. The team also studied 264 healthy families to compare de novo mutations in the genomes of healthy children. The team focused their gene-mutation search on the exome – the small fraction of each person’s genome that encodes proteins, where disease-causing mutations are most likely to occur. Children with and without congenital heart disease had about the same number of de novomutations — on average, slightly less than one protein-altering mutation each. However, the locations of those mutations were markedly different in the two groups. “The mutations in patients with congenital heart disease were found much more frequently in genes that are highly expressed in the developing heart,” Seidman says. The differences became more dramatic when the researchers zeroed in on mutations most likely to impair protein function, such as those that would cause a protein to be cut short. Children with severe congenital heart disease were 7.5 times more likely than healthy children to have a damaging mutation in genes expressed in the developing heart. The researchers found mutations in a variety of genes, but one cellular pathway was markedly enriched in the children with heart defects. That pathway helps regulate gene activity by affecting how DNA is packaged inside cells. The body’s DNA is wrapped around proteins called histones, and chemical tags called methyl groups are added to histones to control which genes are turned on and off. In children with congenital heart disease, the team found an excess of mutations in genes that affect histone methylation at two sites that are known to regulate key developmental genes. Overall, the researchers found that de novo mutations contribute to 10 percent of cases of severe congenital heart disease. Roughly a third of this contribution is from the histone-methylation pathway, Lifton says. He also notes that a mutation in just one copy of a gene in this pathway was enough to markedly increase the risk of a heart defect. Direct sequencing of protein-coding regions of the human genomes to hunt down de novo mutations has only been applied to one other common congenital disease—autism. In that analysis, Lifton and his colleagues at Yale, as well as HHMI investigator Evan Eichler and colleagues at University of Washington, found mutations in some of the same genes mutated in congenital heart disease, and the same histone modification pathway appears to play a major role in autism as well, raising the possibility that this pathway may be perturbed in a variety of congenital disorders, Lifton says. Even if the disease can’t be prevented, identifying the mutations responsible for severe heart defects might help physicians better care for children with congenital heart disease. “After we repair the hearts of these children, some children do great and some do poorly,” Seidman says. Researchers have long suspected that this might be due to differences in the underlying causes of the disease. Understanding those variations might help doctors improve outcomes for their patients. |
 3D computer generated image of chromosomes. Image: cdascher/iStock
3D computer generated image of chromosomes. Image: cdascher/iStock
Every year, thousands of babies are born with severely malformed hearts, disorders known collectively as congenital heart disease. Many of these defects can be repaired though surgery, but researchers don’t understand what causes them or how to prevent them.
Although genetic factors contribute to congenital heart disease, new research shows that about 10 percent of these defects are caused by genetic mutations that are absent in the parents and siblings of affected children, suggesting that new mutations that arise spontaneously—known as de novo mutations—might contribute to the disease.
“Until recently, we simply didn’t have the technology to test for this possibility,” said Richard Lifton, chair of the department of genetics at Yale School of Medicine.
Lifton, who is also a Howard Hughes Medical Institute (HHMI) investigator, together with Christine Seidman, a Harvard Medical School professor of genetics at Brigham and Women’s Hospital, as well as colleagues at Columbia, Mt. Sinai and the University of Pennsylvania, collaborated to study congenital heart disease through the National Heart Lung and Blood Institute’s Pediatric Cardiac Genomics Consortium.
Overall, the researchers found that of the de novo mutations that contribute to 10 percent of severe congenital heart disease cases, roughly a third are from the histone-methylation pathway. Lifton noted that a mutation in just one copy of a gene in this pathway was enough to markedly increase the risk of a heart defect.
Direct sequencing of protein-coding regions of the human genomes to hunt down de novo mutations has only been applied to one other common congenital disease — autism. In that analysis, Lifton and his colleagues at Yale, as well as HHMI investigator Evan Eichler and colleagues at University of Washington, found mutations in some of the same genes mutated in congenital heart disease. The same histone modification pathway appears to play a major role in autism as well, raising the possibility that this pathway may be perturbed in a variety of congenital disorders, Lifton said.
Even if the disease can’t be prevented, identifying the mutations responsible for severe heart defects might help physicians better care for children with congenital heart disease.
“After we repair the hearts of these children, some children do great and some do poorly,” Seidman said.
Researchers have long suspected that this might be due to differences in the underlying causes of the disease. Understanding those variations might help doctors improve outcomes for their patients.
Histone-methylation pathway research
Using robust sequencing technologies developed in recent years, the researchers compared the protein-coding regions of the genomes of children with and without congenital heart disease and their parents, and found that new mutations could explain about 10 percent of severe cases.
The results demonstrated that mutations in several hundred different genes contribute to this trait in different patients, but were concentrated in a pathway that regulates key developmental genes. These genes affect the epigenome, a system of chemical tags that modifies gene expression. The findings were published online in the journal Nature on May 12, 2013.
For the current study, the investigators began with 362 families consisting of two healthy parents with no family history of heart problems and a child with severe congenital heart disease. By comparing genomes within families, they could pinpoint mutations that were present in each child’s DNA, but not in his or her parents.
The team also studied 264 healthy families to compare de novo mutations in the genomes of healthy children.
 Christine SeidmanThe team focused their gene-mutation search on the exome — the small fraction of each person’s genome that encodes proteins, where disease-causing mutations are most likely to occur. Children with and without congenital heart disease had about the same number of de novomutations — on average, slightly less than one protein-altering mutation each. However, the locations of those mutations were markedly different in the two groups.
Christine SeidmanThe team focused their gene-mutation search on the exome — the small fraction of each person’s genome that encodes proteins, where disease-causing mutations are most likely to occur. Children with and without congenital heart disease had about the same number of de novomutations — on average, slightly less than one protein-altering mutation each. However, the locations of those mutations were markedly different in the two groups.
“The mutations in patients with congenital heart disease were found much more frequently in genes that are highly expressed in the developing heart,” said Seidman, who is also an HHMI investigator.
The differences became more dramatic when the researchers zeroed in on mutations most likely to impair protein function, such as those that would cause a protein to be cut short. Children with severe congenital heart disease were 7.5 times more likely than healthy children to have a damaging mutation in genes expressed in the developing heart.
The researchers found mutations in a variety of genes, but one cellular pathway was markedly enriched in the children with heart defects. That pathway helps regulate gene activity by affecting how DNA is packaged inside cells. The body’s DNA is wrapped around proteins called histones, and chemical tags called methyl groups are added to histones to control which genes are turned on and off.
In children with congenital heart disease, the team found an excess of mutations in genes that affect histone methylation at two sites that are known to regulate key developmental genes.
Adapted from HHMI news release.









 The MIT-BIH Polysomnographic Database is a collection of recordings of multiple physiologic signals during sleep. Subjects were monitored in Boston’s Beth Israel Hospital Sleep Laboratory for evaluation of chronic obstructive sleep apnea syndrome, and to test the effects of constant positive airway pressure (CPAP), a standard therapeutic intervention that usually prevents or substantially reduces airway obstruction in these subjects. The database contains over 80 hours’ worth of four-, six-, and seven-channel polysomnographic recordings, each with an ECG signal annotated beat-by-beat, and EEG and respiration signals annotated with respect to sleep stages and apnea. For further information, see
The MIT-BIH Polysomnographic Database is a collection of recordings of multiple physiologic signals during sleep. Subjects were monitored in Boston’s Beth Israel Hospital Sleep Laboratory for evaluation of chronic obstructive sleep apnea syndrome, and to test the effects of constant positive airway pressure (CPAP), a standard therapeutic intervention that usually prevents or substantially reduces airway obstruction in these subjects. The database contains over 80 hours’ worth of four-, six-, and seven-channel polysomnographic recordings, each with an ECG signal annotated beat-by-beat, and EEG and respiration signals annotated with respect to sleep stages and apnea. For further information, see