MONOAMINE, NEUROTROPHIC FACTOR, & PHARMACOKINTIC HYPOTHESES OF DEPRESSION, OLD AND NEWER TREATMENTS
Curator: Zohi Sternberg, PhD
Department of Neurology, University of Buffalo, Baird MS Center, Buffalo, NY.
Depression is the second leading cause of disability worldwide, which struck 20% of women and 15% of men at least one episode in their lifetime. Depression is characterized by two or more weeks of depressed mood or diminished interest, associated with symptoms such as disturbed sleep, decrease in appetite and libido, psychomotor changes, reduced concentration, excessive guilt and suicidal thoughts or attempts.
A variety of genetic, environmental and neurobiological factors are implicated in depression. The genetic contribution to the manifestation of depression has been estimated as 40-50%. However, combinations of multiple genetic factors may be involved in the development of disease, because a defect in a single gene usually fails to induce the expression of multifaceted symptoms of depression. In addition, non-genetic factors such cellular abnormalities and stress, interact with genetic factors, contributing to the prevalence of depression.
Monoamine hypothesis of depression
Monoamine reuptake inhibitors
Among cellular abnormalities contributing to depression is the dysfunction in the monoamine system. The deficiency or imbalances in the monoamine neurotransmitters, such as serotonin, dopamine and norepinephrine has been known to be the cause of depression. Typical antidepressants, such as 5-hydroxytryptamine (5-HT) selective reuptake inhibitors (SSRIs), exert clinical effects by blocking monoamine reuptake by the 5-HT transporter (Fig 1). However, these antidepressants are effective in less than 50% of patients and show a wide spectrum of undesired side effects. In addition, the chronic use of antidepressants is required to observe clinical benefits.
Neurotrophic hypothesis of depression
Although neurotrophic factors are critical signaling molecules for nervous system development, they continue to play an important role in the survival, function and adaptive plasticity of neurons in the adult brain. Of the different families of neurotrophic and/or growth factors expressed in the brain, the most extensively studied in depression is the nerve growth factor (NGF) family, which includes NGF, brain-derived neurotrophic factor (BDNF), and neurotrophin 3 and 4 (NT3 and NT4). Most notable of these has been BDNF and its receptor, tropomyosin-related kinase B (TrkB), a transmembrane receptor with an intracellular tyrosine kinase domain. BDNF–TrkB downstream signaling includes activation of phosphatidyl inositol-3 kinase (PI3K)-Akt (serine threonine kinase or protein kinase B), Ras–mitogen-activated protein kinase (MAPK) and the phospholipaseCg (PLCg)–Ca2+ pathways (Fig 2)
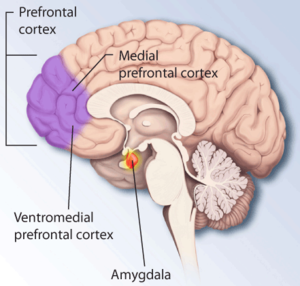
Early studies demonstrated that stress decreases the level of BDNF in the hippocampus. These results, coupled with brain-imaging studies, which reported a decreased volume of limbic brain regions in depressive patients, have led to a neurotrophic hypothesis of depression. Studies show that BDNF has the potential to produce an antidepressant response in behavioral models of depression, and that genetic deletion or blockade of BDNF blocks the effects of antidepressant treatments. However, it is it noteworthy that BDNF has various function depending on the site it is expressed. For example, BDNF in the mesolimbic dopamine system produces prodepressive effects and increases susceptibility to social defeat, effects that could oppose the antidepressant actions of BDNF in the Prefrontal cortex and hippocampus. Interestingly, BDNF administration by routes that would affect multiple brain regions (intracerebroventricular or systemic) produce antidepressant responses.
Furthermore, the deletion or mutation of BDNF results in a state of increased susceptibility to other factors, such as stress. This type of gene-environment interaction is supported by studies demonstrating that BDNF heterozygous deletion mutant mice display depressive behavior only when exposed to mild stress that has no effect in wild-type mice. A chronic treatment with antidepressant is required to induce an increase in BDNF mRNA expression levels. However, it is a matter of debate to whether BDNF underlies the deleterious effects of stress and depression and, conversely, whether induction of BDNF mediates the beneficial effects of antidepressants. Nevertheless, a single nucleotide polymorphism (SNP) of BDNF, Val66Met, provides supporting evidence from human, as well as rodent studies, for a role of BDNF in depressive behavior.

Figure 1. Signaling pathways regulated by chronic antidepressant treatments. Typical antidepressants, such as 5-hydroxytryptamine (5-HT) selective reuptake inhibitors (SSRIs), block monoamine reuptake by the 5-HT transporter (SERT). This leads to regulation of postsynaptic G protein-coupled receptors, which couple to a variety of second messenger systems, including the cAMP–protein kinase A (PKA)–cAMP response element-binding (CREB) pathway [4,6] These effects require chronic SSRI treatment, owing to the requirement for desensitization of 5-HT autoreceptors, and because 5-HT is a neuromodulator that produces slow neuronal responses. By contrast, glutamate produces fast excitation of neurons via stimulation of ionotropic receptors, including AMPA and NMDA receptors, resulting in depolarization and rapid intracellular signaling, such as induction of Ca2+-calmodulin-dependent protein kinase (CAMK). Glutamate and 5-HT signaling lead to regulation of multiple physiological responses, including regulation of synaptic plasticity, as well as gene expression. One target of antidepressant treatment and CREB signaling is brain-derived neurotrophic factor (BDNF). BDNF transcripts may remain in the soma or are targeted for transport to dendrites, where they are subject to activity-dependent translation and release. A common BDNF polymorphism, Val66Met, which is encoded by G196A, blocks the trafficking of BDNF to dendrites. The induction of BDNF and other neurotrophic factors contributes to the actions of antidepressant treatments, including neuroprotection, neuroplasticity and neurogenesis. Abbreviation: SNP, single nucleotide polymorphism
Newer treatments of depression
NMDA receptor antagonists
Typical antidepressants do not increase BDNF release, which could further contribute to the delayed response, as well as limited efficacy of these agents. Furthermore, in patients with severe depression, who are resistant to typical antidepressants, a novel class of antidepressants, the NMDA receptor antagonists, such as ketamine, are being evaluated. This class of antidepressants produces a rapid antidepressant action, an effect not seen with the typical antidepressants. The mechanism of action of NMDA receptor antagonists involves increased glutamate transmission and induction of synaptogenesis, involving the upregulation of BDNF and other neurotrophic factors. The comparison of typical antidepressants with novel, rapid-acting NMDA antagonists also highlights the difference between agents that act on neuromodulatory systems (i.e.monoamines) compared with those that act on the major excitatory neurotransmitter system (i.e.glutamate).
GABA receptor antagonists
Furthermore, gamma amino butyric acid (GABA)-ergic system is known to play a role in mood disorders. GABA system is the prominent inhibitory neurotransmitter in the brain, and a link between GABA(A) receptors and anxiety has been established. However, the role of these receptors in depression has not been validated. GABA(B) receptors, have been also postulated to be involved in the etiology of depression. Studies of GABA(B) receptor antagonists and GABA(B) receptor knockout mice suggest that the blockade, or loss of function of GABA(B) receptors causes an antidepressant-like phenotype. The antidepressant effect of GABA(B) blockade has speculated to be via interacting with the serotonergic system and BDNF. GABA(B) receptor antagonists may represent a new class of antidepressant compounds

Figure 2. Brain-derived neurotrophic factor (BDNF)–tropomyosin-related kinase B (TrkB) signaling pathways. BDNF binding to the extracellular domain of TrkB induces dimerization and activation of the intracellular tyrosine kinase domain. This results in autophosphorylation of tyrosine residues that then serve as sites for interaction with adaptor proteins and activation of intracellular signaling cascades, including the Ras–microtubule-associated protein kinase (MAPK), phosphatidyl inositol-3 kinase (PI3K)/serine threonine kinase (Akt) and phospholipase C (PLC)-g pathways. Phosphorylation of tyrosine 515 of TrkB leads to recruitment of the Src homology 2 domaincontaining (Shc) adaptor protein, followed by recruitment of growth factor receptor-bound protein 2 (Grb2) and son of sevenless (SOS) and activation of the Ras–MAPK pathway (right). Shc–Grb2 can also lead to recruitment of Grb2-associated binder-1 (GAB1) and activation of the PI3K–Akt pathway (left). Phosphorylation of the TrkB tyrosine residue 816 results in recruitment of PLCg, which leads to the formation of inositol triphosphate (IP3) and regulation of intracellular Ca2+ and diacylglycerol (DAG), which activates CAMK and protein kinase C (PKC). These pathways control many different aspects of cellular function, including synaptic plasticity, survival and growth and/or differentiation. Basic and clinical studies demonstrate that BDNF and components of the Ras–MAPK and PI3K–Akt pathways are decreased by stress and depression, and increased by antidepressant treatments. Abbreviations: ERK, extracellular signal regulated kinase; MEK, MAP/ERK kinase; MKP1, MAP kinase phosphatase 1; PDK1, 3-phosphoinositide-dependent protein kinase 1; PTEN, phosphatase and tensin homolog.
Sphingomyelinase /ceramide inhibitors
The lysosomal lipid metabolizing enzyme, acid sphingomyelinase (ASM), cleaves sphingomyelin into ceramide and phosphorylcholine. In a pilot study, the activity of this enzyme was increased in peripheral blood cells of patients with major depressive disorder, making the ASM an interesting molecular target of antidepressant drugs.
It is postulated that the accumulation of the enzyme in the lyzozome may play a role in depressive disorders (pharmacokinetic hypothesis), and its inhibition by cationic amphiphilic substances, which traverse the BBB, and which cause the detachment of the enzyme from the inner lysosomal membranes, and its consecutive inactivation, could improve depressive disorders. In addition, ASM inhibitors could exert antidepressant effects by modulating monoamine receptor and transporter, since ASM inhibitors are known to inhibit interferon-alpha-induced 5-HT uptake.
In addition, ceramide and its metabolite sphingosine-1-phosphate have been shown to also antagonistically regulate apoptosis, cellular differentiation, proliferation and cell migration. Therefore, inhibitors of ASM or ceramide hold promise for a number of new clinical therapies for Alzheimer’s disease and cancer.
Deep brain stimulation
Another new promising method of treating depression, as well as other clinical pathologies such as obsessive-compulsive disorders, Tourette’s syndrome, substance abuse, dementia and anxiety is deep brain stimulation (DBS). These pathologies are classified as the dysfunctions of networks which process motivational and affective stimuli. DBS permits the selective and basically reversible modulation of such networks, with marginal or non adverse effects. In the field of treatment-resistant depressive disorders, uncontrolled studies have been published with initial satisfactory and concordant indications of the therapeutic effect of DBS in a variety of target areas of the brain.
Key words: Depression, Monoamines, NMDA receptor, GABA, Deep brain stimulation, Ceramide, Sphingomyelinase, Cancer, Alzheimer;s diseases
References
1. Albert PR. The neurobiology of depression, revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms. Phil. Trans. R. Soc. B. 2012
2. Lee S. Jeong J. Kwak Y. Park SK. Depression research: where are we now?.[Review] Molecular Brain. 3:8, 2010.
3. Ronald S. Duman and Bhavya Voleti. Signaling pathways underlying the pathophysiology and treatment of depression: novel mechanisms for rapid-acting agents. Trends in Neurosciences January 2012, Vol. 35, No. 1
4. Cryan JF. Slattery DA. GABAB receptors and depression. Current status. [Review] Advances in Pharmacology. 58:427-51, 2010.
5. Schlapfer TE. Kayser S. The development of deep brain stimulation as a putative treatment for resistant psychiatric disorders]. [Review] Nervenarzt. 81(6):696-701, 2010 Jun.
6. Su HC. Ma CT. Lin CF. Wu HT. Chuang YH. Chen LJ. Tsao CW. The acid sphingomyelinase inhibitors block interferon-alpha-induced serotonin uptake via a COX-2/Akt/ERK/STAT-dependent pathway in T cells. International Immunopharmacology. 11(11):1823-31, 2011 Nov.
7. Kornhuber J. Tripal P. Reichel M. Muhle C. Rhein C. Muehlbacher M. Groemer TW. Gulbins E Functional Inhibitors of Acid Sphingomyelinase (FIASMAs): a novel pharmacological group of drugs with broad clinical applications. [Review] Cellular Physiology & Biochemistry. 26(1):9-20, 2010.
8. Kornhuber J. Muehlbacher M. Trapp S. Pechmann S. Friedl A. Reichel M. Muhle C. Terfloth L. Groemer TW. Spitzer GM. Liedl KR. Gulbins E. Tripal P. Identification of novel functional inhibitors of acid sphingomyelinase. PLoS ONE [Electronic Resource]. 6(8):e23852, 2011.
Like this:
Like Loading...
Read Full Post »