English: ATP producing pathways of glucose metabolism in aerobic respiration (Photo credit: Wikipedia)
Author: Larry H. Bernstein, MD, FCAP,
Writer, Author, Responder Clinical Pathologist, Biochemist, and Transfusion Physician _____________________________________________________________________________________________________________________________________________
Heterogeneity The heterogeneity is a problem that will take at least another decade to unravel because of the number of signaling pathways and the crosstalk that is specifically at issue. I must refer back to the work of Frank Dixon, Herschel Sidransky, and others, who did much to develop a concept of neoplasia occurring in several stages – minimal deviation and fast growing. These have differences in growth rates, anaplasia, and biochemical. This resembles the multiple “hit” theory that is described in “systemic inflammatory” disease leading to a final stage, as in sepsis and septic shock.
Tumor heterogeneity is problematic because of differences among the metabolic variety among types of gastrointestinal (GI) cancers, confounding treatment response and prognosis. A group of investigators from Sunnybrook Health Sciences Centre, University of Toronto, Ontario, Canada who evaluated the feasibility and safety of magnetic resonance (MR) imaging–controlled transurethral ultrasound therapy for prostate cancer in humans. Their study’s objective was to prove that using real-time MRI guidance of HIFU treatment is possible and it guarantees that the location of ablated tissue indeed corresponds to the locations planned for treatment. The real-time MRI guidance is an improvement in imaging technology.
The ability to allow resection with removal of the tumor, and adjacent tissue at risk is unproved, and is related to the length of remission.
See comment written for :
Knowing the tumor’s size and location, could we target treatment to THE ROI by applying…..
http://pharmaceuticalintelligence.com/2012/10/16/knowing-the-tumors-size-and-location-could-we-target-treatment-to-the-roi-by-applying-imaging-guided-intervention/
The Response vs. Recurrence Free Interval Conundrum
There is a difference between expected response to esophageal or gastric neoplasms both biologically and in expected response, even given variability within a class. The expected time to recurrence is usually longer in the latter case, but the confounders are –
- age at time of discovery,
- biological time of detection,
- presence of lymph node and/or
- distant metastasis, microscopic vascular invasion.
There is a long latent period in abdominal cancers before discovery, unless a lesion is found incidentally in surgery for another reason. The undeniable reality is that it is not difficult to identify the main lesion, but it is difficult to identify adjacent epithelium that is at risk (transitional or pretransitional). Pathologists have a very good idea about precancerous cervical neoplasia.
The heterogeneity rests within each tumor and between the primary and metastatic sites, which is expected to be improved by targeted therapy directed by tumor-specific testing. Despite rapid advances in our understanding of targeted therapy for GI cancers, the impact on cancer survival has been marginal. Brücher BLDM, Bilchik A, Nissan A, Avital I & Stojadinovic A. Can tumor response to therapy be predicted, thereby improving the selection of patients for cancer treatment? Future Oncology 2012; 8(8): 903-906 , DOI 10.2217/fon.12.78 (doi:10.2217/fon.12.78) The heterogeneity is a problem that will take at least another decade to unravel because of the number of signaling pathways and the crosstalk that is specifically at issue.
Anaerobic Glycolysis and Respiratory Impairment In 1920, Otto Warburg received the Nobel Prize for his work on respiration. He postulated that cancer cells become anaerobic compared with their normal counterpart that uses aerobic respiration to meet most energy needs. He attributed this to “mitochondrial dysfunction. In fact, we now think that in response to oxidative stress, the mitochondrion relies on the Lynen Cycle to make more cells and the major source of energy becomes glycolytic, which is at the expense of the lean body mass (muscle), which produces gluconeogenic precursors from muscle proteolysis (cancer cachexia).
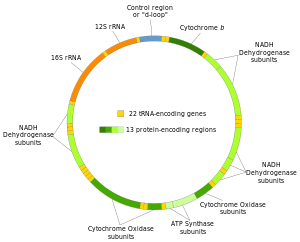
There is a loss of about 26 ATP ~Ps in the transition. The mitochondrial gene expression system includes the mitochondrial genome, mitochondrial ribosomes, and the transcription and translation machinery needed to regulate and conduct gene expression as well as mtDNA replication and repair. Machinery involved in energetics includes the enzymes of the Kreb’s citric acid or TCA (tricarboxylic acid) cycle, some of the enzymes involved in fatty acid catabolism (β-oxidation), and the proteins needed to help regulate these systems. The inner membrane is central to mitochondrial physiology and, as such, contains multiple protein systems of interest. These include the protein complexes involved in the electron transport component of oxidative phosphorylation and proteins involved in substrate and ion transport. ________________________________________________________________________________________________________________________________________________________________________________ Mitochondrial Roles in Cellular Homeostasis Mitochondrial roles in, and effects on, cellular homeostasis extend far beyond the production of ATP, but the transformation of energy is central to most mitochondrial functions. Reducing equivalents are also used for anabolic reactions. The energy produced by mitochondria is most commonly thought of to come from the pyruvate that results from glycolysis, but it is important to keep in mind that the chemical energy contained in both fats and amino acids can also be converted into NADH and FADH2 through mitochondrial pathways.
The major mechanism for harvesting energy from fats is β-oxidation; the major mechanism for harvesting energy from amino acids and pyruvate is the TCA cycle. Once the chemical energy has been transformed into NADH and FADH2 (also discovered by Warburg and the basis for a second Nobel nomination in 1934), these compounds are fed into the mitochondrial respiratory chain. The hydroxyl free radical is extremely reactive. It will react with most, if not all, compounds found in the living cell (including DNA, proteins, lipids and a host of small molecules).
The hydroxyl free radical is so aggressive that it will react within 5 (or so) molecular diameters from its site of production. The damage caused by it, therefore, is very site specific. The reactions of the hydroxyl free radical can be classified as hydrogen abstraction, electron transfer, and addition. The formation of the hydroxyl free radical can be disastrous for living organisms. Unlike superoxide and hydrogen peroxide, which are mainly controlled enzymatically, the hydroxyl free radical is far too reactive to be restricted in such a way – it will even attack antioxidant enzymes. Instead, biological defenses have evolved that reduce the chance that the hydroxyl free radical will be produced and, as nothing is perfect, to repair damage. ________________________________________________________________________________________________________________________________________________________________________________ Oxidative Stress and Mitochondrial Impairment Currently, some endogenous markers are being proposed as useful measures of total “oxidative stress” e.g., 8-hydroxy-2’deoxyguanosine in urine. The ideal scavenger must be non-toxic, have limited or no biological activity, readily reach the site of hydroxyl free radical production (i.e., pass through barriers such as the blood-brain barrier), react rapidly with the free radical, be specific for this radical, and neither the scavenger nor its product(s) should undergo further metabolism. Nitric oxide has a single unpaired electron in its π*2p antibonding orbital and is therefore paramagnetic. This unpaired electron also weakens the overall bonding seen in diatomic nitrogen molecules so that the nitrogen and oxygen atoms are joined by only 2.5 bonds. The structure of nitric oxide is a resonance hybrid of two forms. In living organisms nitric oxide is produced enzymatically. Microbes can generate nitric oxide by the reduction of nitrite or oxidation of ammonia.
In mammals nitric oxide is produced by stepwise oxidation of L-arginine catalyzed by nitric oxide synthase (NOS). Nitric oxide is formed from the guanidino nitrogen of the L-arginine in a reaction that consumes five electrons and requires flavin adenine dinucleotide (FAD), flavin mononucleotide (FMN) tetrahydrobiopterin (BH4), and iron protoporphyrin IX as cofactors. The primary product of NOS activity may be the nitroxyl anion that is then converted to nitric oxide by electron acceptors. The thiol-disulfide redox couple is very important to oxidative metabolism. GSH is a reducing cofactor for glutathione peroxidase, an antioxidant enzyme responsible for the destruction of hydrogen peroxide.
Thiols and disulfides can readily undergo exchange reactions, forming mixed disulfides. Thiol-disulfide exchange is biologically very important. For example, GSH can react with protein cystine groups and influence the correct folding of proteins, and it GSH may play a direct role in cellular signaling through thiol-disulfide exchange reactions with membrane bound receptor proteins (e.g., the insulin receptor complex), transcription factors (e.g., nuclear factor κB), and regulatory proteins in cells. Conditions that alter the redox status of the cell can have important consequences on cellular function. So the complexity of life is not yet unravelled.
_________________________________________________________________________________________________________________________________________________________________________________
Warburgh Effect
Cells seem to be well-adjusted to glycolysis. While Otto Warburg first proposed that cancer cells show increased levels of glucose consumption and lactate fermentation even in the presence of ample oxygen (known as “Warburg Effect”), which requires oxidative phosphorylation to switch to glycolysis promoting the proliferation of cancer cells., many studies have demonstrated glycolysis as the main metabolic pathway in cancer cells. It is now accepted that glycolysis provides cancer cells with the most abundant extracellular nutrient, glucose, to make ample ATP metabolic intermediates, such as ribose sugars, glycerol and citrate, nonessential amino acids, and the oxidative pentose phosphate pathway, which serve as building blocks for cancer cells.
_________________________________________________________________________________________________________________________________________________________________________________
Dampened Mitochondrial Respiration
Since, cancer cells have increased rates of aerobic glycolysis, investigators argue over the function of mitochondria in cancer cells. Mitochondrion, a one of the smaller organelles, produces most of the energy in the form of ATP to supply the body. In Warburg’s theory, the function of cellular mitochondrial respiration is dampened and mitochondria are not fully functional. There are many studies backing this theory. A recent review on hypoxia nicely summarizes some current studies and speculates that the “Warburg Effect” provides a benefit to the tumor not by increasing glycolysis but by decreasing mitochondrial activity.
________________________________________________________________________________________________________________________________________________________________________________
Glycolysis
Glycolysis is enhanced and beneficial to cancer cells. The mammalian target of rapamycin (mTOR) has been well discussed in its role to promote glycolysis; recent literature has revealed some new mechanisms of how glycolysis is promoted during skin cancer development.
On the other hand, Akt is not only involved in the regulation of mitochondrial metabolism in skin cancer but also of glycolysis. Activation of Akt has been found to phosphorylate FoxO3a, a downstream transcription factor of Akt, which promotes glycolysis by inhibiting apoptosis in melanoma. In addition, activated Akt is also associated with stabilized c-Myc and activation of mTOR, which both increase glycolysis for cancer cells.
Nevertheless, ras mutational activation prevails in skin cancer. Oncogenic ras induces glycolysis. In human squamous cell carcinoma, the c-Jun NH(2)-terminal Kinase (JNK) is activated as a mediator of ras signaling, and is essential for ras-induced glycolysis, since pharmacological inhibitors if JNK suppress glycolysis. CD147/basigin, a member of the immunoglobulin superfamily, is high expressed in melanoma and other cancers.
Glyoxalase I (GLO1) is a ubiquitous cellular defense enzyme involved in the detoxification of methylglyoxal, a cytotoxic byproduct of glycolysis. In human melanoma tissue, GLO1 is upregulated at both the mRNA and protein levels.
Knockdown of GLO1 sensitizes A375 and G361 human metastatic melanoma cells to apoptosis.
The transcription factor HIF-1 upregulates a number of genes in low oxygen conditions including glycolytic enzymes, which promotes ATP synthesis in an oxygen independent manner. Studies have demonstrated that hypoxia induces HIF-1 overexpression and its transcriptional activity increases in parallel with the progression of many tumor types. A recent study demonstrated that in malignant melanoma cells, HIF-1 is upregulated, leading to elevated expression of Pyruvate Dehydrogenase Kinase 1 (PDK1), and downregulated mitochondrial oxygen consumption.
The M2 isoform of Pyruvate Kinase (PKM2), which is required for catalyzing the final step of aerobic glycolysis, is highly expressed in cancer cells; whereas the M1 isoform (PKM1) is expressed in normal cells. Studies using the skin cell promotion model (JB6 cells) demonstrated that PKM2 is activated whereas PKM1 is inactivated upon tumor promoter treatment. Acute increases in ROS inhibited PKM2 through oxidation of Cys358 in human lung cancer cells. The levels of ROS and stage of tumor development may be pivotal for the role of PKM2.
_________________________________________________________________________________________________________________________________________________________________________________
Dampening Mitochondrial Both Cause and Effect
Warburg effect is both, a cause and effect of cancer…Review article mentioned in link below explains how different factors can contribute to metabolic reprogramming and Warburg effect….The Supply-based model and Traditional model clearly explains how the cancer cells will progress during different availability of growth factors and nutrients…And recent studies including my project (under process of getting published) will also suggest that growth factors can drive cancer cells to undergo Warburg effect regardless of the presence of oxygen…
Otto Warburg proposed that “EVEN IN THE PRESENCE OF OXYGEN, cancer cells can reprogram their glucose metabolism, and thus their energy production, by limiting their energy metabolism largely to glycolysis” . http://www.ncbi.nlm.nih.gov/pubmed
Metabolic reprogramming: a cancer hallmark even warburg did not anticipate (Ward & Thompson) Posted by Nirav Patel
_______________________________________________________________________________________________________________________________________________________________________________
The autophagic tumor stroma model of cancer metabolism.
Cancer cells induce oxidative stress in adjacent cancer-associated fibroblasts (CAFs). This activates reactive oxygen species (ROS) production and autophagy. ROS production in CAFs, via the bystander eff ect, serves to induce random mutagenesis in epithelial cancer cells, leading to double-strand DNA breaks and aneuploidy. Cancer cells mount an anti-oxidant defense and upregulate molecules that protect them against ROS and autophagy, preventing them from undergoing apoptosis. So, stromal fibroblasts conveniently feed and mutagenize cancer cells, while protecting them against death. See the text for more details. A+, autophagy positive; A-, autophagy negative; AR, autophagy resistant.
1. Recycled Nutrients
2. Random Mutagenesis
3. Protection Against Apoptosis
____________________________________________________________________________________________________________________________________________________________________________
The reverse Warburg effect.
Via oxidative stress, cancer cells activate two major transcription factors in adjacent stromal fibroblasts (hypoxia-inducible factor (HIF)1α and NFκB).
This leads to the onset of both autophagy and mitophagy, as well as aerobic glycolysis, which then produces recycled nutrients (such as lactate, ketones, and glutamine).
These high-energy chemical building blocks can then be transferred and used as fuel in the tricarboxylic acid cycle (TCA) in adjacent cancer cells.
The outcome is high ATP production in cancer cells, and protection against cell death. ROS, reactive oxygen species.
_______________________________________________________________________________________________________________________________________________________________________________
The choline dependent methylation of PP2A is the brake, the “antidote”, which limits “the poison” resulting from an excess of insulin signaling. Moreover, it seems that choline deficiency is involved in the L to M2 transition of PK isoenzymes. The negative regulation of Ras/MAP kinase signals mediated by PP2A phosphatase seems to be complex.
The serine-threonine phosphatase does more than simply counteracting kinases; it binds to the intermediate Shc protein on the signaling cascade, which is inhibited. The targeting of PP2A towards proteins of the signaling pathway depends of the assembly of the different holoenzymes.
The relative decrease of methylated PP2A in the cytosol, not only cancels the brake over the signaling kinases, but also favors the inactivation of PK and PDH, which remain phosphorylated, contributing to the metabolic anomaly of tumor cells. In order to prevent tumors, one should then favor the methylation route rather than the phosphorylation route for choline metabolism.
_________________________________________________________________________________________________________________________________________________________________________________
Martin Canazales observes….
(http://www.cellsignal.com/reference/pathway/warburg_effect.html), is responsible of overactivation of the PI3K…
the produced peroxide via free radicals over activate the cyclooxigenase and consequently the PI3K pathway, thereby activating the most important protein-kinase. This brakes the Warburg effect, and stops the PI3K activation.
(http://www.cellsignal.com/reference/pathway/Akt_PKB.html)
Then all the cancer protein related with the generation of tumor (pAKT,pP70S6K, Cyclin D1, HIF1, VEGF, EGFrc, GSK, Myc, etc, etc, etc) get down regulated. That is what happens when one knocks down the new protein-kinase in pancreatic cancer cell lines. These pancreatic cancer cell lines divide very-very-very slowly.
_________________________________________________________________________________________________________________________________________________________________________________
I now transition from what is understood about the metabolic signatures of cancer that tend to behave more alike than the cell of origin, but not initially. This is perhaps a key to therapeutics. >>>
Time of intervention>>> and right intervention.
_________________________________________________________________________________________________________________________________________________________________________________
Can tumor response to therapy be predicted, thereby improving the selection of patients for cancer treatment? The goal is not just complete response. Histopathological response seems to be related post-treatment histopathological assessment but it is not free from the challenge of accurately determining treatment response, as this method cannot delineate whether or not there are residual cancer cells. Functional imaging to assess metabolic response by 18-fluorodeoxyglucose PET also has its limits, as the results are impacted significantly by several variables:
- tumor type
- sizing
- doubling time
- anaplasia?
- extent of tumor necrosis
- presence of tumor at the margin of biopsy
- lymph node and/or distant metastasis
- vascular involvement
- type of antitumor therapy and the time when response was determined.
The new modality should be based on individualized histopathology as well as tumor molecular, genetic and functional characteristics, and individual patients’ characteristics, a greater challenge in an era of ‘minimally invasive treatment’. This has been pointed out by Brücher et al. if the International Consortium on Cancer with respect to the shortcoming of MIS as follows: Minimally Invasive Surgery (MIS) vs. conventional surgery dissection applied to cancer tissue with the known pathophysiology of recurrence and remission cycles has its short term advantages.
- in many cases MIS is not the right surgical decision
- predicting the uncertain future behavior of the tumor with respect to its response to therapeutics bears uncertain outcomes.
An increase in the desirable outcomes of MIS as a modality of treatment, will be assisted in the future, when anticipated progress is made in the field of
- Cancer Research,
- Translational Medicine and
- Personalized Medicine,
when each of the cancer types, above, will already have a Genetic Marker allowing the Clinical Team to use the marker(s) for:
- prediction of Patient’s reaction to Drug induction
- design of Clinical Trials to validate drug efficacy on small subset of patients predicted to react favorable to drug regimen, increasing validity and reliability
- Genetical identification of patients at no need to have a drug administered if non sensitivity to the drug has been predicted by the genetic marker.
See listing of cancers provided by Dr. Aviva Lev-Ari.
Lev-Ari A. Personalized Medicine: Cancer Cell Biology and Minimally Invasive Surgery (MIS). ________________________________________________________________________________________________________________________________________________________________________________ See comment:
Judging the ‘Tumor response’-there is more food for thought
That is an optimistic order to effectively carry out in the face of the statistical/mathematical challenge imposed for any real success.
Brücher BLDM, Bilchik A, Nissan A, Avital I & Stojadinovic A. Can tumor response to therapy be predicted, thereby improving the selection of patients for cancer treatment? Future Oncology 2012; 8(8): 903-906 , DOI 10.2217/fon.12.78 (doi:10.2217/fon.12.78) _________________________________________________________________________________________________________________________________________________________________________________ A Model Based on Kullback Entropy and Identifying and Classifying Anomalies This listing suggests that for every cancer the following data has to be collected (except doubling time). If there are 8 variables, the classification based on these alone would calculate to be very sizable based on Eugene Rypka’s feature extraction and classification. But looking forward,
Treatment for cure is not the endpoint, but the best that can be done is to extend the time of survival to a realistic long term goal and retain a quality of life. Brücher BLDM, Piso P, Verwaal V et al. Peritoneal carcinomatosis: overview and basics. Cancer Invest.30(3),209–224 (2012). Brücher BLDM, Swisher S, Königsrainer A et al. Response to preoperative therapy in upper gastrointestinal cancers. Ann. Surg. Oncol.16(4),878–886 (2009). Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer47(1),207–214 (1981). Therasse P, Arbuck SG, Eisenhauer EA et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J. Natl Cancer Inst.92(3),205–216 (2000). Brücher BLDM, Becker K, Lordick F et al. The clinical impact of histopathological response assessment by residual tumor cell quantification in esophageal squamous cell carcinomas. Cancer106(10),2119–2127 (2006). _________________________________________________________________________________________________________________________________________________________________________________
The critical question encountered by the pathologist is that key histological stains have been used for some time, such as Her2, and a number of others to establish tumor cell type, and differences with cell types. The number will grow as the genomic identifiers are explored and put to use. It doesn’t appear that the pathologist will be displaced any time soon. This is separate from older observations of nuclear polymorphism, anaplastic changes related to cell adhesion, etc. These do not displace the information gained from staging criteria. Clearly, there is much information that is used for individual decisions about therapeutic approach, which will undergo further refinement even before the end of this decade.
_________________________________________________________________________________________________________________________________________________________________________________ Melanoma Example A marker for increased glycolysis in melanoma is the elevated levels of Lactate Dehydrogenase (LDH) in the blood of patients with melanoma, which has proven to be an accurate predictor of prognosis and response to treatments. LDH converts pyruvate, the final product of glycolysis, to lactate when oxygen is absent. High concentrations of lactate, in turn, negatively regulate LDH. Therefore, targeting acid excretion may provide a feasible and effective therapeutic approach for melanoma. For instance, JugloSne, a main active component in walnut, has been used in traditional medicines.
Studies have shown that Juglone causes cell membrane damage and increased LDH levels in a concentration-dependent manner in cultured melanoma cells. As one of the rate-limiting enzyme of glycolysis, 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase isozyme 3 (PFKFB3) is activated in neoplastic cells. Studies have confirmed that an inhibitor of PFKFB3, 3-(3-pyridinyl)-1-(4-pyridinyl)-2-propen-1-one (3PO), suppresses glycolysis in neoplastic cells. In melanoma cell lines, the concentrations of Fru-2, 6-BP, lactate, ATP, NAD+, and NADH are diminished by 3PO. Therefore, targeting PFKFB3 using 3PO and other PFKFB3 specific inhibitors could be effective in melanoma chemotherapy.
This is only one example of the encouraging results from targeted therapy. An unexplored idea was provided to me that is interesting and be highly conditional, by loading with high concentrations of ketones to offset the glycolytic pathway redirected bypass of mitochondrial pathways. There is an inherent problem with muscle proteolysis raising the glucose level from gluconeogenesis. The effect is uncertain with respect to TCA cycle intermediates. It seems plausible that cure is not necessarily attainable due to inability to identify portions of proximate local tumor, modification and drug resistance. The reliable extension of disease free survival and maintaining a patient acceptable quality of life is improvable. __________________________________________________________________________________________________________________________________________________________________________________
Ward PS, Thompson CB. Metabolic Reprogramming: A Cancer Hallmark Even Warburg Did Not Anticipate. Cancer Cell. 2012; 21(3):297-308.
- Quiescent versus Proliferating Cells: Both Use Mitochondria, but to Different Ends
- Altered Metabolism Is a Direct Response to Growth-Factor Signaling
- PI3K/Akt/mTORC1 Activation: Driving Anabolic Metabolism and Tumorigenesis by Reprogramming Mitochondria
 Bhowmick NA. Metastatic Ability: Adapting to a Tissue Site Unseen. Cancer Cell 2012; 22(5): 563-564. _____________________________________________________________________________________________________________________________________________________________________________ Therapeutic strategies that target glycolysis and biosynthetic pathways in cancer cells are currently the main focus of research in the field of cancer metabolism. In this issue of Cancer Cell, Hitosugi and colleagues show that targeting PGAM1 could be a way of “killing two birds with one stone”. Chaneton B, Gottlieb E. PGAMgnam Style: A Glycolytic Switch Controls Biosynthesis. Cancer Cell 2012; 22(5): 565-566. ______________________________________________________________________________________________________________________________________________________________________________ The Polycomb epigenetic silencing protein EZH2 is affected by gain-of-function somatic mutations in B cell lymphomas. Two recent reports describe the development of highly selective EZH2 inhibitors and reveal mutant EZH2 as playing an essential role in maintaining lymphoma proliferation. EZH2 inhibitors are thus a promising new targeted therapy for lymphoma. Melnick A. Epigenetic Therapy Leaps Ahead with Specific Targeting of EZH2. Cancer Cell 22(5): 569-570. _______________________________________________________________________________________________________________________________________________________________________________ The microenvironment of the primary as well as the metastatic tumor sites can determine the ability for a disseminated tumor to progress. In this issue of Cancer Cell, Calon and colleagues find that systemic TGF-β can facilitate colon cancer metastatic engraftment and expansion. Calon A, Espinet E, Palomo-Ponce S, Tauriello DVF, et al. Dependency of Colorectal Cancer on a TGF-β-Driven Program in Stromal Cells for Metastasis Initiation. Cancer Cell 2012;22(5): 571-584.
Bhowmick NA. Metastatic Ability: Adapting to a Tissue Site Unseen. Cancer Cell 2012; 22(5): 563-564. _____________________________________________________________________________________________________________________________________________________________________________ Therapeutic strategies that target glycolysis and biosynthetic pathways in cancer cells are currently the main focus of research in the field of cancer metabolism. In this issue of Cancer Cell, Hitosugi and colleagues show that targeting PGAM1 could be a way of “killing two birds with one stone”. Chaneton B, Gottlieb E. PGAMgnam Style: A Glycolytic Switch Controls Biosynthesis. Cancer Cell 2012; 22(5): 565-566. ______________________________________________________________________________________________________________________________________________________________________________ The Polycomb epigenetic silencing protein EZH2 is affected by gain-of-function somatic mutations in B cell lymphomas. Two recent reports describe the development of highly selective EZH2 inhibitors and reveal mutant EZH2 as playing an essential role in maintaining lymphoma proliferation. EZH2 inhibitors are thus a promising new targeted therapy for lymphoma. Melnick A. Epigenetic Therapy Leaps Ahead with Specific Targeting of EZH2. Cancer Cell 22(5): 569-570. _______________________________________________________________________________________________________________________________________________________________________________ The microenvironment of the primary as well as the metastatic tumor sites can determine the ability for a disseminated tumor to progress. In this issue of Cancer Cell, Calon and colleagues find that systemic TGF-β can facilitate colon cancer metastatic engraftment and expansion. Calon A, Espinet E, Palomo-Ponce S, Tauriello DVF, et al. Dependency of Colorectal Cancer on a TGF-β-Driven Program in Stromal Cells for Metastasis Initiation. Cancer Cell 2012;22(5): 571-584. 
_______________________________________________________________________________________________________________________________________________________________________________ An analysis of what is possible, but who knows how far into the accelerating future? Tumor response criteria: are they appropriate? The International Consortium is centered at the Billroth Institute, in Munich. Interesting it is that Billroth was the father of abdominal surgery and performed the first esophagectomy and the firat gastrectomy. He also pioneered in keeping a record of treatments and outcomes in the 19th century, which Halsted studied. I need not repeat what has been stated in the post. The pathologist’s role is still important, as the editorial in Future Oncology gets at. This also requires necessary and sufficient features to extract differentiating classifiers. I don’t think we shall see pathologists the likes of many who were masters until the 1990′s. The surgical pathologist today cannot have complete command of the large knowledge base, but the tumor registry and the cancer committee has evolved to a better stage than in the 1960′s. Surgical grand rounds have been used for teaching and evaluating the practice since at least the 1960′s. What is asked is that we go beyond that.
See comment written for:
Knowing the tumor’s size and location, could we target treatment to THE ROI by applying…..
http://pharmaceuticalintelligence.com/2012/10/16/knowing-the-tumors-size-and-location-could-we-target-treatment-to-the-roi-by-applying-imaging-guided-intervention/
________________________________________________________________________________________________________________________________________________________________________________ Evidence-based medicine Evidence-based medicine is substantially flawed because of reliance on meta-analysis to arrive at conclusions from underpowered and inconsistent studies, discarding more than half of the studies examined that don’t meet the inclusion criteria.
- – There can be no movement forward without the systematic collection of data into a functionally well designed repository.
- – The current construct of the EMR probably has to be “remodeled” if not “remade”.
- – The studies will have to use real data, not aggregates of studies with “missing information”.
- – Bioinformatics is an emerging field that is only supported in the top two tiers of academic medical centers, which would include the well known cancer centers in Boston, Houston, and New York.
I don’t place much hope in “Watson” coming to the rescue, because you have to collect both a lot of information and “sufficient” information.
- -”Sufficient” information has been precluded by years of cost-elimination without paying attention to the real impact of “technologies” on costs, and an inherent competition between labor and “capital” investment.
- – Despite the progress in genomics, the heterogeneity of these solid tumors is a natural adaptation that occurs in carcinogenesis.
- The heterogeneity traced over a time-span should have information about stage in carcinogenesis.
- The pathologist can see and interpret histologic grades in the evolution that may have a better relationship to the evolutionary studies of genomics and signaling pathways than to stage of disease, but by combining the best available evidence, you move to a better classification. Without good classification, I don’t see how you can arrive at “science based” personalized medicine.
–there is still a Rubicon to cross in going from genomics to translational medicine, which extends to diet and lifestyle.
Search Results for ‘cancer’ on this web site
Cancer Genomics – Leading the Way by Cancer Genomics Program at UC Santa Cruz Closing the gap towards real-time, imaging-guided treatment of cancer patients. Lipid Profile, Saturated Fats, Raman Spectrosopy, Cancer Cytology
mRNA interference with cancer expression
Pancreatic cancer genomes: Axon guidance pathway genes – aberrations revealed Biomarker tool development for Early Diagnosis of Pancreatic Cancer: Van Andel Institute and Emory University
Is the Warburg Effect the cause or the effect of cancer: A 21st Century View?
Crucial role of Nitric Oxide in Cancer Targeting Glucose Deprived Network Along with Targeted Cancer Therapy Can be a Possible Method of Treatment
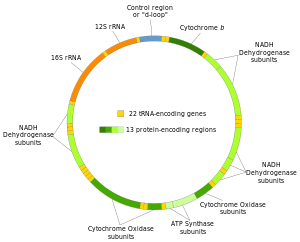
Structure of the human mitochondrial genome. (Photo credit: Wikipedia)

English: ATP production in aerobic respiration (Photo credit: Wikipedia)
00
Like this:
Like Loading...
Read Full Post »


 Bhowmick NA.
Bhowmick NA.