UPDATED on 3/14/2022 – Call for the abandonment of the Off-pump CABG surgery (OPCAB) in the On-pump / Off-pump Debate, +100 Research Studies
Curator: Aviva Lev-Ari, PhD, RN
UPDATED on 3/14/2022
Debate over? On-pump CABG, off-pump CABG lead to similar 10-year outcomes
Surgeons have debated for 20 years over which method is better—traditional on-pump surgery (which uses an extracorporeal membrane oxygenation [ECMO] heart-lung machine to circulate and oxygenate the the blood while the heart is stopped) or off-pump, which eliminates complications potentially caused by ECMO but makes the procedure more technically difficult. Monitoring the post-CABG outcomes of all original ROOBY trial patients, this phase IV clinical trial represents the largest U.S.-based, multi-center, randomized clinical trial comparing off-pump versus on-pump patients.
The researchers tracked more than 1,000 veterans treated with on-pump procedures and more than 1,000 veterans treated with off-pump procedures over 10 years. These veterans are a national cohort from 18 VA Centers. The average age at the time of surgery for both groups was about 63 years old.
Mortality similar for on-pump vs off-pump CABG
According to the authors, no significant 10-year treatment-related differences were documented for any primary or secondary post-CABG endpoint rates. Endpoints included repeat CABG, other heart revascularization procedures, and changes in cardiac symptoms. The death rates at 10 years were 34.2 percent for the off-pump group and 31.1 for the on-pump group.
Although the 10-year outcome rates were not different, the researchers did document a slightly shorter revascularization-free survival period among patients in the off-pump group. Additionally, the median time to death in the off-pump patients was 5.6 years, and the median time to death in the on-pump patients was 6.1 years. Across all study outcomes, moreover, no off-pump advantages were found.
The analyses for cardiac outcomes for these two groups were completed from May 2017 to December 2021.
“While our findings may not settle the ongoing debate about on-pump versus off-pump advantages with CABG, the data is strong to support the notion that for patients who are viable candidates for either procedure, no benefits were found for using an off-pump procedure,” lead author Laurie Shroyer, PhD, professor of surgery in the Renaissance School of Medicine at Stony Brook University and Northport Veteran Affairs (VA) Medical Center WOC Health Science Officer, said in a statement. “As these veterans were nearly all men, the findings should not be generalized to women or non-veterans. Thus, surgeons should choose the best CABG method based each individual patient’s risks and in light of the surgeon’s own technical CABG expertise and post-CABG outcome experiences. In summary, each CABG patient’s care should be customized to meet their unique needs.”
The study authors write that the findings in their report do concur with the 2015 consensus statement by the International Society for Minimally Invasive Cardiothoracic Surgery.[2] That consensus statement says off-pump CABG may be associated with an increased long-term risk of reintervention and death. Yet, the authors found “10-year symptomatic benefit of patients who underwent CABG was not influenced by the treatment approach.”
“These operations were performed at a time when this revascularization approach was considered novel, and it served as an impetus for a few dedicated surgeons to advance it further to become a minimally invasive robotic and often hybrid operation,” Thomas V. Bilfinger, MD, a professor of cardiothoracic surgery at the Renaissance School of Medicine who was not involved in the study, said in the same statement. “While it is good to know there is no difference in the long-term outcomes between off and on pump groups, the lasting importance of this research is that it provides a seed to newer procedural developments that will lead to long-lasting beneficial outcomes for today’s patients.”
References:
Related CABG Content:
Still No. 1: CABG outperforms FFR-PCI when treating CAD
New ACC/AHA guidelines detail updated recommendations for PCI, CABG
CABG still the ‘treatment of choice’ for patients with complex three-vessel CAD
PCI and CABG for left main CAD associated with similar all-cause mortality rates
@@@@
The curator shadowed Dr. J. Walker @MGH performing On-pump CABG in 1/2005 and On-pump CABG performed @Texas Heart Institute in 2/2005, and attended demos of ECMO at Vanderbilt Medical Center, Department of Surgery, Perfusion Program, 8/2005
Public release date: 22-Jul-2013
Contact: Gina Orlando
gina.orlando@bmc.org
617-638-8490
Boston University Medical Center
BMC surgeon recommends off-pump coronary artery bypass grafting be abandoned
(Boston) – In a Special Report in the current issue of Circulation, Boston Medical Center cardiothoracic surgeon Harold Lazar, MD, has found that off-pump coronary artery bypass graft (OPCAB) surgery has failed to show any significant improvement in short-term morbidity or mortality as compared to the traditional on-pump coronary artery bypass graft (CABG) surgery. He recommends that the technique be abandoned, unless surgeons who perform off-pump surgery can show that their own results are as good as results reported with the traditional on-pump surgery.
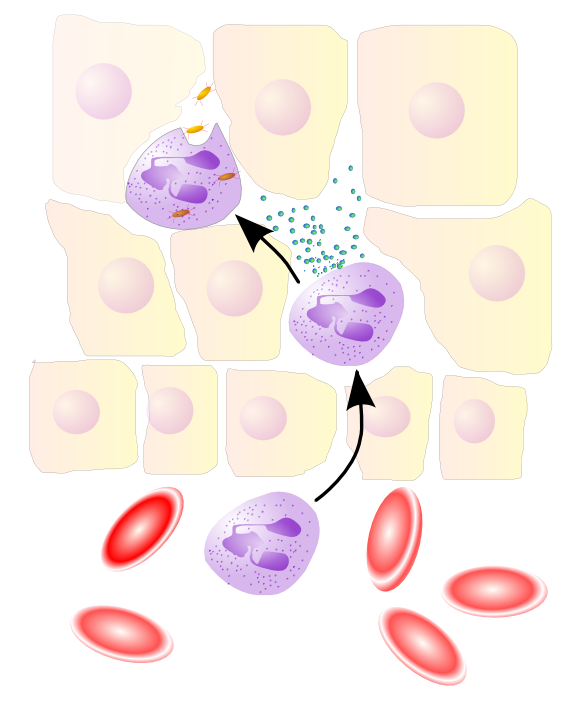
During off-pump coronary artery bypass graft surgery, the heart is still beating while the graft attachments are made to bypass a blockage. While performing on-pump CABG surgery, the heart is stopped and a heart-lung machine takes over the work for the heart and lungs. This method has been an effective, safe and time-proven technique and is considered the gold standard with which all other surgical revascularization methods have been compared. However, performing coronary revascularization this way can result in myocardial ischemic injury, neurocognitive deficits, and strokes and activate inflammatory pathways that contribute to pulmonary, renal and hematologic complications.
In order to accurately compare the advantages and disadvantages of OPCAB and to determine what, if any, role it should have in the practice of surgical coronary artery revascularization, Lazar examined clinical data from numerous studies worldwide and found the OPCAB technique had failed to show any significant improvement in short-term morbidity or mortality.
According to Lazar a major impetus for performing OPCAB was to avoid the possible detrimental effects of cardiopulmonary bypass, which include activation of inflammatory pathways, changes in neurological and cognitive function and alterations in quality of life. “However, patients undergoing OPCAB have not shown any benefits in these areas,” said Lazar, a professor of surgery at Boston University School Medicine. “Even in those studies in which OPCAB has resulted in a small improvement in early postoperative outcomes, these improvements are no longer apparent on long-term follow-up,” he added.
In fact, several studies suggest that long-term survival may be significantly reduced in OPCAB patients compared with patients in whom on-pump techniques were used. Lazar explains that this may be attributable to the significant increase in incomplete revascularization seen in OPCAB patients and may be responsible for the increase in recurrent angina and need for revascularization procedures seen in OPCAB patients.
“Unless individual surgeons can demonstrate that they can achieve short- and long-term outcomes with OPCABG that are comparable to on-pump CABG results, they should abandon this technique,” said Lazar.
The debate over abandoning off-pump CABG surgery
JULY 29, 2013 Michael O’Riordan
In the July 23, 2013 issue of Circulation, Dr Harold Lazar (Boston Medical Center, MA) argues that the primary focus of surgical coronary revascularization is complete revascularization and a technically perfect anastomosis that uses the best conduits with a minimal amount of hemodynamic instability. He adds that the procedure should be able to be performed “under all circumstances, on all patients, at all institutions, regardless of their cardiac volume.
“We must not forget that patients are sent for surgical revascularization because medical management has failed, their cardiologists believe that stents will not result in complete revascularization, and the goal is for optimal long-term survival and enhanced freedom from recurrent angina and the need for [repeat] revascularization,” writes Lazar. “These goals can be best achieved with on-pump CABG surgery.”
Dr Robbin Cohen (University of Southern California, LA), on the other hand, said that many physicians are routine off-pump CABG surgeons and the data suggest that results achieved by experienced operators are excellent. It is also a cheaper operation in experienced hands. He does not believe that OPCAB should be abandoned but acknowledged there is a need to better identify the ideal patient who would benefit from the procedure.
While there is yet no consensus and no studies have identified subgroups with better results, the ideal OPCAB candidate is one with a severely diseased descending aorta and those with single-vessel or two-vessel disease—in other words, a patient with favorable anatomy that doesn’t require moving the heart around too much, he said.
“I don’t doubt that I have treated some patients with off-pump surgery where if I had put them on the pump I would have killed them,” Cohen told heartwire.
Looking at the big picture
In his perspective, Lazar analyzes previously published retrospective studies and prospective, randomized controlled clinical trials, including the Randomized On/Off Bypass (ROOBY), Smart Management of Arterial Revascularization Therapy (SMART), and Coronary Artery Bypass Surgery Off- or On-Pump Revascularization (CORONARY) studies.
In ROOBY, the primary short-term end point of death and major cardiovascular events at 30 days was similar in the on-pump and off-pump treatment arms, while cardiac-related mortality and major adverse events were higher in the OPCAB arm at one year. The SMART trial also failed to show a mortality benefit with OPCAB. The CORONARY investigators reported no difference in the composite of death, nonfatal cerebrovascular accidents, nonfatal MIs, or new renal failure requiring dialysis between OPCAB and on-pump CABG surgery. In CORONARY, there was also no difference in quality-of-life scores and neurocognitive function at one year.
Importantly, Lazar says the data from published meta-analyses show that OPCAB patients tend to receive fewer grafts and have a higher incidence of incomplete revascularization. “Despite advances in stabilizers and other equipment, it may be difficult to graft inferior and posterolateral vessels because of right and left ventricular distension and hemodynamic changes,” he writes.
Abandoned? Not so fast, says another expert
So, will OPCAB be abandoned? Not likely, says Cohen. OPCAB is performed often in other countries, mainly because the procedure is quicker and has lower costs than conventional CABG surgery. Cohen had high praise for the systematic review by Lazar, however, noting that the OPCAB vs on-pump CABG debate is a complicated topic and nearly each month brings a new review, journal article, or other analysis in the medical journals.
“Early on, most of us assumed that the morbidity associated with cardiac surgery, that being stroke, renal failure, and so on, was the result of cardiopulmonary bypass,” said Cohen. “And when we started doing off-pump procedures, we assumed that the morbidity would be eliminated. That wasn’t the case. Some of the early studies showed an advantage with blood use and sometimes with the utilization of resources, but morbidity and mortality with the two surgeries were the same.”
Cohen addressed the criticism that OPCAB provides incomplete revascularization compared with on-pump CABG and that the anastomoses are not as good, saying these are all valid criticisms of the procedure. He agreed with Lazar’s point that if surgeons must cross over from OPCAB to conventional bypass, the outcomes are poor. To date, however, OPCAB “has been a moving target,” he added, noting that there has been a move toward addressing these shortcomings.
At one point, Cohen said his group was performing up to 90% of cardiac surgeries with OPCAB but now do just 10% of procedures off-pump. The reasons for decline in use include all of the previously cited reasons:
- incomplete revascularization,
- poorer anastomoses, and
- no reduction in morbidity and mortality to show it is better than conventional CABG, as well the fact that
- it is difficult to teach to residents.
For OPCAB to move forward, he said that research needs to provide evidence that the procedure is as least as effective and as durable as on-pump CABG. There is also a need to identify specific patient subgroups that would benefit from OPCAB, such as
- older patients, those with
- existing renal failure, or
- patients who have previously had a stroke.
Source
Related links
- Off-pump/on-pump CABG: Still no consensus
[Interventional/Surgery > Interventional/Surgery; Mar 11, 2013] - CORONARY analysis: High-risk patients do better with off-pump CABG
[Interventional/Surgery > Interventional/Surgery; Nov 03, 2012] - CORONARY: Off-pump and on-pump CABG give similar short-term outcomes
[Interventional/Surgery > Interventional/Surgery; Mar 26, 2012] - New data suggest off-pump CABG has higher mortality than on-pump
[Interventional/Surgery > Interventional/Surgery; Oct 03, 2011] - Short-term benefits of off-pump bypass surgery off-set by long-term risks in Beijing study
[Interventional/Surgery > Interventional/Surgery; Apr 27, 2010] - Off-pump CABG shows no benefit over on-pump approach: ROOBY study
[Interventional/Surgery > Interventional/Surgery; Nov 04, 2009]
| Lazar and Cohen report no conflicts of interest. |
REVIEWS in
http://www.ncbi.nlm.nih.gov/pubmed?linkname=pubmed_pubmed_reviews&from_uid=23877063
Should off-pump coronary artery bypass grafting be abandoned?
Lazar HL.
Circulation. 2013 Jul 23;128(4):406-13. doi: 10.1161/CIRCULATIONAHA.113.003388. No abstract available.
- PMID: 23877063 [PubMed – in process]
Off-pump coronary artery bypass grafting: simple concept but potentially sublime scientific value.
Ngaage DL.
Med Sci Monit. 2004 Mar;10(3):RA47-54. Epub 2004 Mar 1. Review.
- PMID: 14976442 [PubMed – indexed for MEDLINE]
Salzberg SP, Adams DH, Filsoufi F.
Curr Opin Cardiol. 2005 Nov;20(6):509-16. Review.
- PMID: 16234622 [PubMed – indexed for MEDLINE]
Outcomes of off-pump coronary artery bypass surgery: current best available evidence.
Raja SG, Berg GA.
Indian Heart J. 2007 Jan-Feb;59(1):15-27. Review.
- PMID: 19098331 [PubMed – indexed for MEDLINE]
Off-pump coronary artery bypass grafting through sternotomy: for whom?
Noora J, Puskas JD.
Curr Opin Cardiol. 2006 Nov;21(6):573-7. Review.
- PMID: 17053406 [PubMed – indexed for MEDLINE]
Reoperative off-pump coronary artery bypass grafting: current outcomes, concerns and controversies.
Raja SG, Amrani M.
Expert Rev Cardiovasc Ther. 2010 May;8(5):685-94. doi: 10.1586/erc.10.14. Review.
- PMID: 20450302 [PubMed – indexed for MEDLINE]
Off-pump versus on-pump coronary artery bypass grafting.
Halkos ME, Puskas JD.
Surg Clin North Am. 2009 Aug;89(4):913-22, ix. doi: 10.1016/j.suc.2009.06.015. Review.
Raja SG.
Curr Cardiol Rev. 2012 Feb;8(1):26-36. Review.
- PMID: 22845813 [PubMed – indexed for MEDLINE] Free PMC Article
Current status of off-pump coronary artery bypass surgery.
Raja SG, Dreyfus GD.
Asian Cardiovasc Thorac Ann. 2008 Apr;16(2):164-78. Review.
- PMID: 18381881 [PubMed – indexed for MEDLINE]
Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease.
Møller CH, Penninga L, Wetterslev J, Steinbrüchel DA, Gluud C.
Cochrane Database Syst Rev. 2012 Mar 14;3:CD007224. doi: 10.1002/14651858.CD007224.pub2. Review.
- PMID: 22419321 [PubMed – indexed for MEDLINE]
REFERENCES in
http://www.ncbi.nlm.nih.gov/pubmed
1.
Should off-pump coronary artery bypass grafting be abandoned?
Lazar HL.
Circulation. 2013 Jul 23;128(4):406-13. doi: 10.1161/CIRCULATIONAHA.113.003388. No abstract available.
PMID: 23877063 [PubMed – in process]
Select item 14762348
2.
Sharony R, Grossi EA, Saunders PC, Galloway AC, Applebaum R, Ribakove GH, Culliford AT, Kanchuger M, Kronzon I, Colvin SB.
J Thorac Cardiovasc Surg. 2004 Feb;127(2):406-13.
PMID: 14762348 [PubMed – indexed for MEDLINE]
Select item 14752427
3.
Mack MJ, Pfister A, Bachand D, Emery R, Magee MJ, Connolly M, Subramanian V.
J Thorac Cardiovasc Surg. 2004 Jan;127(1):167-73.
PMID: 14752427 [PubMed – indexed for MEDLINE]
Select item 12324731
4.
Tschernko EM, Bambazek A, Wisser W, Partik B, Jantsch U, Kubin K, Ehrlich M, Klimscha W, Grimm M, Keznickl FP.
J Thorac Cardiovasc Surg. 2002 Oct;124(4):732-8.
PMID: 12324731 [PubMed – indexed for MEDLINE]
Select item 14976442
5.
Off-pump coronary artery bypass grafting: simple concept but potentially sublime scientific value.
Ngaage DL.
Med Sci Monit. 2004 Mar;10(3):RA47-54. Epub 2004 Mar 1. Review.
PMID: 14976442 [PubMed – indexed for MEDLINE]
Select item 18455592
6.
Chowdhury UK, Malik V, Yadav R, Seth S, Ramakrishnan L, Kalaivani M, Reddy SM, Subramaniam GK, Govindappa R, Kakani M.
J Thorac Cardiovasc Surg. 2008 May;135(5):1110-9, 1119.e1-10. doi: 10.1016/j.jtcvs.2007.12.029.
PMID: 18455592 [PubMed – indexed for MEDLINE]
Select item 19185140
7.
Angelini GD, Culliford L, Smith DK, Hamilton MC, Murphy GJ, Ascione R, Baumbach A, Reeves BC.
J Thorac Cardiovasc Surg. 2009 Feb;137(2):295-303. doi: 10.1016/j.jtcvs.2008.09.046.
PMID: 19185140 [PubMed – indexed for MEDLINE] Free PMC Article
Select item 12086378
8.
Beating heart versus conventional reoperative coronary artery bypass surgery.
Mishra Y, Wasir H, Kohli V, Meharwal ZS, Bapna R, Mehta Y, Trehan N.
Indian Heart J. 2002 Mar-Apr;54(2):159-63.
PMID: 12086378 [PubMed – indexed for MEDLINE]
Select item 22436550
9.
Mishra YK, Mishra M, Malhotra R, Meharwal ZS, Kohli V, Trehan N.
Innovations (Phila). 2005 Winter;1(2):88-91. doi: 10.1097/01.imi.0000189937.33748.19.
PMID: 22436550 [PubMed]
Select item 16863772
10.
Mishra M, Malhotra R, Karlekar A, Mishra Y, Trehan N.
Ann Thorac Surg. 2006 Aug;82(2):608-14.
PMID: 16863772 [PubMed – indexed for MEDLINE]
Select item 18249555
11.
Yu HY, Li JY, Sun S, Hung KY, Wang JL, Chen YS, Wang SS, Lin FY.
Eur J Cardiothorac Surg. 2008 Mar;33(3):364-9. doi: 10.1016/j.ejcts.2007.12.027. Epub 2008 Feb 4.
PMID: 18249555 [PubMed – indexed for MEDLINE]
Select item 11565659
12.
Off-pump bypass grafting is safe in patients with left main coronary disease.
Dewey TM, Magee MJ, Edgerton JR, Mathison M, Tennison D, Mack MJ.
Ann Thorac Surg. 2001 Sep;72(3):788-91; discussion 792.
PMID: 11565659 [PubMed – indexed for MEDLINE]
Select item 15276508
13.
Velissaris T, Tang AT, Murray M, Mehta RL, Wood PJ, Hett DA, Ohri SK.
Ann Thorac Surg. 2004 Aug;78(2):506-12; discussion 506-12.
PMID: 15276508 [PubMed – indexed for MEDLINE]
Select item 12698142
14.
Puskas JD, Williams WH, Duke PG, Staples JR, Glas KE, Marshall JJ, Leimbach M, Huber P, Garas S, Sammons BH, McCall SA, Petersen RJ, Bailey DE, Chu H, Mahoney EM, Weintraub WS, Guyton RA.
J Thorac Cardiovasc Surg. 2003 Apr;125(4):797-808.
PMID: 12698142 [PubMed – indexed for MEDLINE]
Select item 16733171
15.
Relationship between atrial histopathology and atrial fibrillation after coronary bypass surgery.
Mariscalco G, Engström KG, Ferrarese S, Cozzi G, Bruno VD, Sessa F, Sala A.
J Thorac Cardiovasc Surg. 2006 Jun;131(6):1364-72.
PMID: 16733171 [PubMed – indexed for MEDLINE]
Select item 14666033
16.
Scarborough JE, White W, Derilus FE, Mathew JP, Newman MF, Landolfo KP; Neurological Outcome Research Group.
J Thorac Cardiovasc Surg. 2003 Nov;126(5):1561-7.
PMID: 14666033 [PubMed – indexed for MEDLINE]
Select item 16305860
17.
Chukwuemeka A, Weisel A, Maganti M, Nette AF, Wijeysundera DN, Beattie WS, Borger MA.
Ann Thorac Surg. 2005 Dec;80(6):2148-53.
PMID: 16305860 [PubMed – indexed for MEDLINE]
Select item 21051050
18.
Is off-pump coronary artery bypass grafting superior to conventional bypass in octogenarians?
LaPar DJ, Bhamidipati CM, Reece TB, Cleveland JC, Kron IL, Ailawadi G.
J Thorac Cardiovasc Surg. 2011 Jan;141(1):81-90. doi: 10.1016/j.jtcvs.2010.09.012. Epub 2010 Nov 4.
PMID: 21051050 [PubMed – indexed for MEDLINE] Free PMC Article
Select item 17258568
19.
Sajja LR, Mannam G, Chakravarthi RM, Sompalli S, Naidu SK, Somaraju B, Penumatsa RR.
J Thorac Cardiovasc Surg. 2007 Feb;133(2):378-88. Epub 2007 Jan 16.
PMID: 17258568 [PubMed – indexed for MEDLINE]
Select item 14752428
20.
Wu Y, Grunkemeier GL, Handy JR Jr.
J Thorac Cardiovasc Surg. 2004 Jan;127(1):174-8.
PMID: 14752428 [PubMed – indexed for MEDLINE]
Select item 21529848
21.
Ben-Gal Y, Stone GW, Smith CR, Williams MR, Weisz G, Stewart AS, Takayama H, Genereux P, Argenziano M.
J Thorac Cardiovasc Surg. 2011 Aug;142(2):e33-9. doi: 10.1016/j.jtcvs.2011.03.022. Epub 2011 Apr 29.
PMID: 21529848 [PubMed – indexed for MEDLINE]
Select item 16482929
22.
Manabe S, Arai H, Tanaka H, Tabuchi N, Sunamori M.
Jpn J Thorac Cardiovasc Surg. 2006 Jan;54(1):3-10.
PMID: 16482929 [PubMed – indexed for MEDLINE]
Select item 16234622
23.
Salzberg SP, Adams DH, Filsoufi F.
Curr Opin Cardiol. 2005 Nov;20(6):509-16. Review.
PMID: 16234622 [PubMed – indexed for MEDLINE]
Select item 15063246
24.
Bucerius J, Gummert JF, Walther T, Schmitt DV, Doll N, Falk V, Mohr FW.
Ann Thorac Surg. 2004 Apr;77(4):1250-6.
PMID: 15063246 [PubMed – indexed for MEDLINE]
Select item 19098331
25.
Outcomes of off-pump coronary artery bypass surgery: current best available evidence.
Raja SG, Berg GA.
Indian Heart J. 2007 Jan-Feb;59(1):15-27. Review.
PMID: 19098331 [PubMed – indexed for MEDLINE]
Select item 23084105
26.
Keeling WB, Kilgo PD, Puskas JD, Halkos ME, Lattouf OM, Guyton RA, Thourani VH.
J Thorac Cardiovasc Surg. 2012 Oct 16. doi:pii: S0022-5223(12)01147-6. 10.1016/j.jtcvs.2012.09.035. [Epub ahead of print]
PMID: 23084105 [PubMed – as supplied by publisher]
Select item 16305858
27.
Perioperative patency of coronary artery bypass grafting is not influenced by off-pump technique.
Onorati F, Olivito S, Mastroroberto P, di Virgilio A, Esposito A, Perrotti A, Renzulli A.
Ann Thorac Surg. 2005 Dec;80(6):2132-40.
PMID: 16305858 [PubMed – indexed for MEDLINE]
Select item 22002967
28.
Bayram H, Erer D, Iriz E, Zor MH, Gulbahar O, Ozdogan ME.
Perfusion. 2012 Jan;27(1):56-64. doi: 10.1177/0267659111424639. Epub 2011 Oct 14.
PMID: 22002967 [PubMed – indexed for MEDLINE]
Select item 20447041
29.
Reber D, Brouwer R, Buchwald D, Fritz M, Germing A, Lindstaedt M, Klak K, Laczkovics A.
Artif Organs. 2010 Mar;34(3):179-84. doi: 10.1111/j.1525-1594.2009.00836.x.
PMID: 20447041 [PubMed – indexed for MEDLINE]
Select item 16740529
30.
Al-Ruzzeh S, George S, Bustami M, Wray J, Ilsley C, Athanasiou T, Amrani M.
BMJ. 2006 Jun 10;332(7554):1365. Epub 2006 Jun 1.
PMID: 16740529 [PubMed – indexed for MEDLINE] Free PMC Article
Select item 12902131
31.
Takanashi S, Fukui T, Hosoda Y, Shimizu Y.
Ann Thorac Surg. 2003 Aug;76(2):635-7.
PMID: 12902131 [PubMed – indexed for MEDLINE]
Select item 12698147
32.
Aydin NB, Gercekoglu H, Aksu B, Ozkul V, Sener T, Kiygil I, Turkoglu T, Cimen S, Babacan F, Demirtas M.
J Thorac Cardiovasc Surg. 2003 Apr;125(4):843-8.
PMID: 12698147 [PubMed – indexed for MEDLINE]
Select item 11544625
33.
Progression to 100% off-pump coronary artery bypass with the Octopus 1 dual holder.
Roy A, Stanbridge RL, O’Regan D, Salerno G, Saldanha C, Griselli M, Cherian A.
Heart Surg Forum. 2001;4(2):174-8.
PMID: 11544625 [PubMed – indexed for MEDLINE]
Select item 20083683
34.
Møller CH, Perko MJ, Lund JT, Andersen LW, Kelbaek H, Madsen JK, Winkel P, Gluud C, Steinbrüchel DA.
Circulation. 2010 Feb 2;121(4):498-504. doi: 10.1161/CIRCULATIONAHA.109.880443. Epub 2010 Jan 18.
PMID: 20083683 [PubMed – indexed for MEDLINE] Free Article
Select item 22036259
35.
Elmistekawy E, Chan V, Bourke ME, Dupuis JY, Rubens FD, Mesana TG, Ruel M.
J Thorac Cardiovasc Surg. 2012 Jan;143(1):85-92. doi: 10.1016/j.jtcvs.2011.09.035. Epub 2011 Oct 27.
PMID: 22036259 [PubMed – indexed for MEDLINE]
Select item 15173734
36.
Abu-Omar Y, Balacumaraswami L, Pigott DW, Matthews PM, Taggart DP.
J Thorac Cardiovasc Surg. 2004 Jun;127(6):1759-65.
PMID: 15173734 [PubMed – indexed for MEDLINE]
Select item 15172262
37.
Kamiya H, Watanabe G, Takemura H, Tomita S, Nagamine H, Kanamori T.
Ann Thorac Surg. 2004 Jun;77(6):2046-50.
PMID: 15172262 [PubMed – indexed for MEDLINE]
Select item 15561032
38.
Off-pump coronary artery bypass grafting in patients with renal dysfunction.
Tabata M, Takanashi S, Fukui T, Horai T, Uchimuro T, Kitabayashi K, Hosoda Y.
Ann Thorac Surg. 2004 Dec;78(6):2044-9.
PMID: 15561032 [PubMed – indexed for MEDLINE]
Select item 16142517
39.
Diabetes in patients undergoing coronary artery bypass grafting. Impact on perioperative outcome.
Bucerius J, Gummert JF, Walther T, Doll N, Barten MJ, Falk V, Mohr FW.
Z Kardiol. 2005 Sep;94(9):575-82.
PMID: 16142517 [PubMed – indexed for MEDLINE]
Select item 17053406
40.
Off-pump coronary artery bypass grafting through sternotomy: for whom?
Noora J, Puskas JD.
Curr Opin Cardiol. 2006 Nov;21(6):573-7. Review.
PMID: 17053406 [PubMed – indexed for MEDLINE]
Select item 17384571
41.
Crescenzi G, Landoni G, Romano A, Boroli F, Giardina G, Bignami E, Fochi O, Aletti G, Rosica C, Zangrillo A.
Minerva Anestesiol. 2007 Mar;73(3):135-41.
PMID: 17384571 [PubMed – indexed for MEDLINE] Free Article
Select item 17014446
42.
Donne AJ, Waterman P, Crawford L, Balaji HP, Nigam A.
Clin Otolaryngol. 2006 Oct;31(5):381-5.
PMID: 17014446 [PubMed – indexed for MEDLINE]
Select item 20450302
43.
Reoperative off-pump coronary artery bypass grafting: current outcomes, concerns and controversies.
Raja SG, Amrani M.
Expert Rev Cardiovasc Ther. 2010 May;8(5):685-94. doi: 10.1586/erc.10.14. Review.
PMID: 20450302 [PubMed – indexed for MEDLINE]
Select item 16399291
44.
Clinical outcomes of nonelective coronary revascularization with and without cardiopulmonary bypass.
Stamou SC, Hill PC, Haile E, Prince S, Mack MJ, Corso PJ.
J Thorac Cardiovasc Surg. 2006 Jan;131(1):28-33.
PMID: 16399291 [PubMed – indexed for MEDLINE]
Select item 21281950
45.
Misfeld M, Brereton RJ, Sweetman EA, Doig GS.
J Thorac Cardiovasc Surg. 2011 Aug;142(2):e11-7. doi: 10.1016/j.jtcvs.2010.11.034. Epub 2011 Feb 1.
PMID: 21281950 [PubMed – indexed for MEDLINE]
Select item 18805269
46.
Li Y, Zheng Z, Hu S.
J Thorac Cardiovasc Surg. 2008 Sep;136(3):657-64. doi: 10.1016/j.jtcvs.2007.12.069. Epub 2008 Jul 26.
PMID: 18805269 [PubMed – indexed for MEDLINE]
Select item 16307999
47.
Parolari A, Mussoni L, Frigerio M, Naliato M, Alamanni F, Polvani GL, Agrifoglio M, Veglia F, Tremoli E, Biglioli P, Camera M.
J Thorac Cardiovasc Surg. 2005 Dec;130(6):1561-6.
PMID: 16307999 [PubMed – indexed for MEDLINE]
Select item 16153906
48.
Ruel M, Suuronen EJ, Song J, Kapila V, Gunning D, Waghray G, Rubens FD, Mesana TG.
J Thorac Cardiovasc Surg. 2005 Sep;130(3):633-9.
PMID: 16153906 [PubMed – indexed for MEDLINE]
Select item 22523305
49.
Houlind K, Kjeldsen BJ, Madsen SN, Rasmussen BS, Holme SJ, Nielsen PH, Mortensen PE; DOORS Study Group.
Circulation. 2012 May 22;125(20):2431-9. doi: 10.1161/CIRCULATIONAHA.111.052571. Epub 2012 Apr 20.
PMID: 22523305 [PubMed – indexed for MEDLINE] Free Article
Select item 17588377
50.
Kai M, Hanyu M, Soga Y, Nomoto T, Nakano J, Matsuo T, Umehara E, Kawato M, Okabayashi H.
Ann Thorac Surg. 2007 Jul;84(1):32-6.
PMID: 17588377 [PubMed – indexed for MEDLINE]
Select item 17703615
51.
[Coronary artery bypass grafting in patients with dialysis-dependent renal failure].
Mizumoto T, Adachi K, Hatanaka K, Sakamoto R, Seko H, Nakanishi R, Kinoshita T, Fujii H.
Kyobu Geka. 2007 Aug;60(9):785-9; discussion 790-3. Japanese.
PMID: 17703615 [PubMed – indexed for MEDLINE]
Select item 19379976
52.
Surgical volume and outcomes of off-pump coronary artery bypass graft surgery: Does it matter?
Konety SH, Rosenthal GE, Vaughan-Sarrazin MS.
J Thorac Cardiovasc Surg. 2009 May;137(5):1116-23.e1. doi: 10.1016/j.jtcvs.2008.12.038. Epub 2009 Mar 25.
PMID: 19379976 [PubMed – indexed for MEDLINE]
Select item 19782844
53.
Off-pump versus on-pump coronary artery bypass grafting.
Halkos ME, Puskas JD.
Surg Clin North Am. 2009 Aug;89(4):913-22, ix. doi: 10.1016/j.suc.2009.06.015. Review.
PMID: 19782844 [PubMed – indexed for MEDLINE]
Select item 15224025
54.
Casati V, Della Valle P, Benussi S, Franco A, Gerli C, Baili P, Alfieri O, D’Angelo A.
J Thorac Cardiovasc Surg. 2004 Jul;128(1):83-91.
PMID: 15224025 [PubMed – indexed for MEDLINE]
Select item 10881825
55.
Stroke in octogenarians undergoing coronary artery surgery with and without cardiopulmonary bypass.
Ricci M, Karamanoukian HL, Abraham R, Von Fricken K, D’Ancona G, Choi S, Bergsland J, Salerno TA.
Ann Thorac Surg. 2000 May;69(5):1471-5.
PMID: 10881825 [PubMed – indexed for MEDLINE]
Select item 23335652
56.
Scrascia G, Rotunno C, Guida P, Conte M, Amorese L, Margari V, Schinosa Lde L, Paparella D.
Interact Cardiovasc Thorac Surg. 2013 May;16(5):636-42. doi: 10.1093/icvts/ivs525. Epub 2013 Jan 18.
PMID: 23335652 [PubMed – in process] Free Article
Select item 22845813
57.
Raja SG.
Curr Cardiol Rev. 2012 Feb;8(1):26-36. Review.
PMID: 22845813 [PubMed – indexed for MEDLINE] Free PMC Article
Select item 16286278
58.
Aydin NB, Sener T, Kehlibar IK, Turkoglu T, Karpuzoglu OE, Ozkul V, Gercekoglu H.
Heart Surg Forum. 2005;8(6):E456-61; discussion E461.
PMID: 16286278 [PubMed – indexed for MEDLINE]
Select item 9768998
59.
Minimally invasive coronary artery bypass grafting: port-access approach versus off-pump techniques.
Reichenspurner H, Boehm DH, Welz A, Schmitz C, Wildhirt S, Schulze C, Meiser B, Schütz A, Reichart B.
Ann Thorac Surg. 1998 Sep;66(3):1036-40.
PMID: 9768998 [PubMed – indexed for MEDLINE]
Select item 17888966
60.
Hammon JW, Stump DA, Butterworth JF, Moody DM, Rorie K, Deal DD, Kincaid EH, Oaks TE, Kon ND.
Ann Thorac Surg. 2007 Oct;84(4):1174-8; discussion 1178-9.
PMID: 17888966 [PubMed – indexed for MEDLINE]
Select item 15236490
61.
Zhu YB, Xu JP, Liu ZY, Yang DN, Li XD, Li HY.
J Zhejiang Univ Sci. 2004 Aug;5(8):1005-8.
PMID: 15236490 [PubMed – indexed for MEDLINE]
Select item 9769005
62.
Off-pump multivessel coronary bypass via sternotomy is safe and effective.
Puskas JD, Wright CE, Ronson RS, Brown WM 3rd, Gott JP, Guyton RA.
Ann Thorac Surg. 1998 Sep;66(3):1068-72.
PMID: 9769005 [PubMed – indexed for MEDLINE]
Select item 18329466
63.
Nakano J, Okabayashi H, Hanyu M, Soga Y, Nomoto T, Arai Y, Matsuo T, Kai M, Kawatou M.
J Thorac Cardiovasc Surg. 2008 Mar;135(3):540-5. doi: 10.1016/j.jtcvs.2007.11.008.
PMID: 18329466 [PubMed – indexed for MEDLINE]
Select item 18329463
64.
Miyahara K, Matsuura A, Takemura H, Saito S, Sawaki S, Yoshioka T, Ito H.
J Thorac Cardiovasc Surg. 2008 Mar;135(3):521-6. doi: 10.1016/j.jtcvs.2007.10.006.
PMID: 18329463 [PubMed – indexed for MEDLINE]
Select item 18329465
65.
Balacumaraswami L, Abu-Omar Y, Selvanayagam J, Pigott D, Taggart DP.
J Thorac Cardiovasc Surg. 2008 Mar;135(3):533-9. doi: 10.1016/j.jtcvs.2007.10.027.
PMID: 18329465 [PubMed – indexed for MEDLINE]
Select item 18381881
66.
Current status of off-pump coronary artery bypass surgery.
Raja SG, Dreyfus GD.
Asian Cardiovasc Thorac Ann. 2008 Apr;16(2):164-78. Review.
PMID: 18381881 [PubMed – indexed for MEDLINE]
Select item 21421501
67.
[Circulating endothelial cell injury in on-pump and off-pump coronary-artery bypass grafting].
SONG TN, GAO BR, ZHAO QM.
Nan Fang Yi Ke Da Xue Xue Bao. 2011 Mar;31(3):535-8. Chinese.
PMID: 21421501 [PubMed – indexed for MEDLINE] Free Article
Select item 17599498
68.
Ballotta A, Saleh HZ, El Baghdady HW, Gomaa M, Belloli F, Kandil H, Balbaa Y, Bettini F, Bossone E, Menicanti L, Frigiola A, Bellucci C, Mehta RH.
J Thorac Cardiovasc Surg. 2007 Jul;134(1):132-8.
PMID: 17599498 [PubMed – indexed for MEDLINE]
Select item 14752424
69.
Equivalent midterm outcomes after off-pump and on-pump coronary surgery.
Sabik JF, Blackstone EH, Lytle BW, Houghtaling PL, Gillinov AM, Cosgrove DM.
J Thorac Cardiovasc Surg. 2004 Jan;127(1):142-8.
PMID: 14752424 [PubMed – indexed for MEDLINE]
Select item 23597624
70.
Outcomes of off-pump versus on-pump coronary artery bypass grafting: Impact of preoperative risk.
Polomsky M, He X, O’Brien SM, Puskas JD.
J Thorac Cardiovasc Surg. 2013 May;145(5):1193-8. doi: 10.1016/j.jtcvs.2013.02.002.
PMID: 23597624 [PubMed – indexed for MEDLINE]
Select item 17670644
71.
Emergency conversion in off-pump coronary artery bypass grafting.
Tabata M, Takanashi S, Horai T, Fukui T, Hosoda Y.
Interact Cardiovasc Thorac Surg. 2006 Oct;5(5):555-9. Epub 2006 Jun 15.
PMID: 17670644 [PubMed] Free Article
Select item 19379995
72.
Sokal A, Zembala M, Radomski A, Kocher A, Pacholewicz J, Los J, Jedrzejczyk E, Zembala M, Radomski M.
J Thorac Cardiovasc Surg. 2009 May;137(5):1218-24. doi: 10.1016/j.jtcvs.2008.11.004. Epub 2009 Feb 23.
PMID: 19379995 [PubMed – indexed for MEDLINE]
Select item 18815649
73.
Yoo KJ, Kim HO, Kwak YL, Kang SM, Jang YS, Lim SH, Hwang KC, Cho SW, Yang YS, Li RK, Kim BS.
Can J Surg. 2008 Aug;51(4):269-75.
PMID: 18815649 [PubMed – indexed for MEDLINE] Free PMC Article
Select item 20971248
74.
Suzuki T, Asai T, Matsubayashi K, Kambara A, Hiramatsu N, Kinoshita T, Nishimura O.
Ann Thorac Surg. 2010 Nov;90(5):1501-6. doi: 10.1016/j.athoracsur.2010.06.023.
PMID: 20971248 [PubMed – indexed for MEDLINE]
Select item 11565657
75.
Magee MJ, Dewey TM, Acuff T, Edgerton JR, Hebeler JF, Prince SL, Mack MJ.
Ann Thorac Surg. 2001 Sep;72(3):776-80; discussion 780-1.
PMID: 11565657 [PubMed – indexed for MEDLINE]
Select item 11279409
76.
Ascione R, Williams S, Lloyd CT, Sundaramoorthi T, Pitsis AA, Angelini GD.
J Thorac Cardiovasc Surg. 2001 Apr;121(4):689-96.
PMID: 11279409 [PubMed – indexed for MEDLINE]
Select item 12078783
77.
Chamberlain MH, Ascione R, Reeves BC, Angelini GD.
Ann Thorac Surg. 2002 Jun;73(6):1866-73.
PMID: 12078783 [PubMed – indexed for MEDLINE]
Select item 11603449
78.
Off-pump coronary artery bypass grafting decreases risk-adjusted mortality and morbidity.
Cleveland JC Jr, Shroyer AL, Chen AY, Peterson E, Grover FL.
Ann Thorac Surg. 2001 Oct;72(4):1282-8; discussion 1288-9.
PMID: 11603449 [PubMed – indexed for MEDLINE]
Select item 22419321
79.
Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease.
Møller CH, Penninga L, Wetterslev J, Steinbrüchel DA, Gluud C.
Cochrane Database Syst Rev. 2012 Mar 14;3:CD007224. doi: 10.1002/14651858.CD007224.pub2. Review.
PMID: 22419321 [PubMed – indexed for MEDLINE]
Select item 19559187
80.
Raja SG, Siddiqui H, Ilsley CD, Amrani M.
Ann Thorac Surg. 2009 Jul;88(1):47-52. doi: 10.1016/j.athoracsur.2009.04.013.
PMID: 19559187 [PubMed – indexed for MEDLINE]
Select item 22197616
81.
Off-pump bilateral skeletonized internal thoracic artery grafting in elderly patients.
Kinoshita T, Asai T, Suzuki T, Kuroyanagi S, Hosoba S, Takashima N.
Ann Thorac Surg. 2012 Feb;93(2):531-6. doi: 10.1016/j.athoracsur.2011.09.077. Epub 2011 Dec 23.
PMID: 22197616 [PubMed – indexed for MEDLINE]
Select item 12902081
82.
Al-Ruzzeh S, Athanasiou T, George S, Glenville BE, DeSouza AC, Pepper JR, Amrani M.
Ann Thorac Surg. 2003 Aug;76(2):444-51; discussion 451-2.
PMID: 12902081 [PubMed – indexed for MEDLINE]
Select item 22154798
83.
Lemma MG, Coscioni E, Tritto FP, Centofanti P, Fondacone C, Salica A, Rossi A, De Santo T, Di Benedetto G, Piazza L, Rinaldi M, Schinosa AL, De Paulis R, Contino M, Genoni M.
J Thorac Cardiovasc Surg. 2012 Mar;143(3):625-31. doi: 10.1016/j.jtcvs.2011.11.011. Epub 2011 Dec 10.
PMID: 22154798 [PubMed – indexed for MEDLINE]
Select item 15854936
84.
Weerasinghe A, Athanasiou T, Al-Ruzzeh S, Casula R, Tekkis PP, Amrani M, Punjabi P, Taylor K, Stanbridge R, Glenville B.
Ann Thorac Surg. 2005 May;79(5):1577-83.
PMID: 15854936 [PubMed – indexed for MEDLINE]
Select item 16967324
85.
Scherer M, Sirat AS, Dogan S, Aybek T, Moritz A, Wimmer-Greinecker G.
Cardiovasc Eng. 2006 Sep;6(3):118-21.
PMID: 16967324 [PubMed – indexed for MEDLINE]
Select item 18245699
86.
Off-pump coronary artery bypass grafting in left ventricular dysfunction.
Masoumi M, Saidi MR, Rostami F, Sepahi H, Roushani D.
Asian Cardiovasc Thorac Ann. 2008 Jan;16(1):16-20.
PMID: 18245699 [PubMed – indexed for MEDLINE]
Select item 10536955
87.
Diegeler A, Matin M, Falk V, Binner C, Walther T, Autschbach R, Mohr FW.
Eur J Cardiothorac Surg. 1999 Sep;16 Suppl 1:S79-82.
PMID: 10536955 [PubMed – indexed for MEDLINE]
Select item 15223396
88.
Trainees operating on high-risk patients without cardiopulmonary bypass: a high-risk strategy?
Ascione R, Reeves BC, Pano M, Angelini GD.
Ann Thorac Surg. 2004 Jul;78(1):26-33.
PMID: 15223396 [PubMed – indexed for MEDLINE]
Select item 9262597
89.
Coronary artery bypass grafting “on pump”: role of three-day discharge.
Ott RA, Gutfinger DE, Miller MP, Selvan A, Codini MA, Alimadadian H, Tanner TM.
Ann Thorac Surg. 1997 Aug;64(2):478-81.
PMID: 9262597 [PubMed – indexed for MEDLINE]
Select item 15784358
90.
Is cardiopulmonary bypass a reason for aspirin resistance after coronary artery bypass grafting?
Zimmermann N, Kurt M, Wenk A, Winter J, Gams E, Hohlfeld T.
Eur J Cardiothorac Surg. 2005 Apr;27(4):606-10. Epub 2005 Jan 19.
PMID: 15784358 [PubMed – indexed for MEDLINE]
Select item 15063245
91.
Karthik S, Musleh G, Grayson AD, Keenan DJ, Pullan DM, Dihmis WC, Hasan R, Fabri BM.
Ann Thorac Surg. 2004 Apr;77(4):1245-9.
PMID: 15063245 [PubMed – indexed for MEDLINE]
Select item 12538138
92.
Off-pump coronary artery bypass surgery–initial experience in Gdansk: a brief review.
Keita L, Anisimowicz L.
Heart Surg Forum. 2002;5(3):240-2.
PMID: 12538138 [PubMed – indexed for MEDLINE]
Select item 12202877
93.
Improved outcomes in coronary artery bypass grafting with beating-heart techniques.
Mack M, Bachand D, Acuff T, Edgerton J, Prince S, Dewey T, Magee M.
J Thorac Cardiovasc Surg. 2002 Sep;124(3):598-607.
PMID: 12202877 [PubMed – indexed for MEDLINE]
Select item 16399302
94.
Hammon JW, Stump DA, Butterworth JF, Moody DM, Rorie K, Deal DD, Kincaid EH, Oaks TE, Kon ND.
J Thorac Cardiovasc Surg. 2006 Jan;131(1):114-21. Epub 2005 Dec 9.
PMID: 16399302 [PubMed – indexed for MEDLINE]
Select item 14635411
95.
[Right heart support during coronary artery bypass grafting without cardiopulmonary bypass].
Fernández AL, Tamayo E, Echevarría JR, Hernando MJ, Cubero T, Agudado MJ, López G.
Rev Med Univ Navarra. 2003 Apr-Jun;47(2):14-7. Spanish.
PMID: 14635411 [PubMed – indexed for MEDLINE]
Select item 22698600
96.
Ten-year outcome analysis of off-pump sequential grafting: single surgeon, single center experience.
Raja SG, Salhiyyah K, Navaratnarajah M, Rafiq MU, Felderhof J, Walker CP, Ilsley CD, Amrani M.
Heart Surg Forum. 2012 Jun;15(3):E136-42. doi: 10.1532/HSF98.20111087.
PMID: 22698600 [PubMed – indexed for MEDLINE]
Select item 23430415
97.
Monitoring brain oxygen saturation during awake off-pump coronary artery bypass.
Toda A, Watanabe G, Matsumoto I, Tomita S, Yamaguchi S, Ohtake H.
Asian Cardiovasc Thorac Ann. 2013 Feb;21(1):14-21. doi: 10.1177/0218492312444908.
PMID: 23430415 [PubMed – in process]
Select item 9671898
98.
Jansen EW, Borst C, Lahpor JR, Gründeman PF, Eefting FD, Nierich A, Robles de Medina EO, Bredée JJ.
J Thorac Cardiovasc Surg. 1998 Jul;116(1):60-7.
PMID: 9671898 [PubMed – indexed for MEDLINE]
Select item 15282460
99.
Does off-pump total arterial grafting increase the incidence of intraoperative graft failure?
Balacumaraswami L, Abu-Omar Y, Anastasiadis K, Choudhary B, Pigott D, Yeong SK, Taggart DP.
J Thorac Cardiovasc Surg. 2004 Aug;128(2):238-44.
PMID: 15282460 [PubMed – indexed for MEDLINE]
Select item 22436497
100.
Routine off-pump coronary artery bypass: reasons for on-pump conversion.
Hirose H, Amano A.
Innovations (Phila). 2005 Fall;1(1):28-31.
PMID: 22436497 [PubMed]
Select item 18637191
101.
Uva MS, Matias F, Cavaco S, Magalhães MP.
Trials. 2008 Jul 17;9:44. doi: 10.1186/1745-6215-9-44.
PMID: 18637191 [PubMed] Free PMC Article