Vascular Repair: Stents and Biologically Active Implants
This is the second article of a three part series recognizing the immense contribution of Elazer Edelman, MD, PhD, and his laboratory group at MIT to vascular biology, cardiovascular disease studies, and the bioengineering, development, and use of stenting technology for drug delivery, vascular repair, and limitation of vessel damage caused by stent placement.
The effects of stent placement on vascular injury and the initiation of an inflammatory response
Leukocytes are recruited early and abundantly to experimentally injured vessels,
- in direct proportion to cell proliferation and intimal growth.
- markers of restenosis risk in patients undergoing angioplasty.
- signal leukocyte recruitment and function, thereby
- promote intimal growth
- M1/70, an anti-CD11b blocking mAb, was administered to rabbits before, and every 48 hr for 3, 6, or 14 days after iliac artery balloon denudation.
- M1/70 was bound to isolated rabbit monocytes.
The result was
- Mac-1-mediated dose-dependent
- inhibition of fibrinogen binding in vitro, thereby,
- reducing by half leukocyte recruitment at 3, 6, and 14 days after injury.
- 0.32+0.08 mm2 in vehicle treated controls, P<0.01, and
- 0.38+0.08mm2 in IgG-treated controls, P<0.005;
- 0.84+ 0.13 mm2 in vehicle-treated controls, P <0.05, and
- 0.90+0.15 mm2 in IgG-treated controls, P <0.02).
- leukocyte recruitment to and
- infiltration of injured arteries
may be a valid target for preventing intimal hyperplasia. (1) Emerging data indicate that the inflammatory response after mechanical arterial injury
- correlates with the severity of neointimal hyperplasia in animal models
- and post angioplasty restenosis in humans.
- stimulation of the innate immune system,
- induced in close temporal proximity to the vascular injury,
- would modulate the results of the procedure.
- serum interleukin-1 levels, and
- monocytic stimulation (CD14 levels on monocytes)
- 1.7+1.2% of total cells in controls and
- 4.2+1.8% in LPS-treated rabbits (n=4, P<0.05).
- luminal stenosis: 38+4.2% versus 23+2.6%, mean+SEM; n=8, P<0.05; and
- neointima-to-media ratio: 1.26+0.21 versus 0.66+0.09, P<0.05 in LPS-treated animals compared with controls.
- in correlation with the severity of intimal hyperplasia.
- LPS treatment increased neointimal area after stenting
- from 0.57+0.07 to 0.77+0.1 mm2, and
- stenosis from 9+1% to 13+1.7% (n=5, P<0.05).
- concurrently with arterial vascular injury
- facilitates neointimal formation, and conditions associated with
- increased inflammation may increase restenosis.(2)
- to reduce their risk for in-stent restenosis.
- arterial drug deposition,
- distribution, and
- retention.
- computational fluid dynamics and
- transient drug diffusion–convection.
- empiric data from stented porcine coronary arteries.
- efficiently delivered nearly continuous drug levels, but
- the slow rate of drug presentation limited arterial drug uptake.
- the rates of drug release and absorption matched,
- which occurred for hour-long drug release.
- modulation of drug concentration potently impacts
- the magnitude of arterial drug deposition,
- while changes in coating drug mass affect duration of release.
- in governing arterial drug uptake and suggest
- novel drug delivery strategies for controlling spatio-temporal arterial drug distribution.(3)
- Drug-eluting stents were implanted into porcine coronary arteries, arterial drug uptake was followed and modeled using 2-dimensional computational drug transport.
- an alternate, mechanism for rapid transport has been proposed involving carrier-mediated transport.
- arterial drug deposition varied by up to 114% two weeks after stent implantation.
- extent of adherent mural thrombus fluctuated by 113% within 3 days.
- elevate arterial drug deposition in proportion to the thrombus size
- by reducing drug washout subsequently increasing local drug availability.
http://dx. doi.org/10.1016/j.jconrel.2007.06.025.
Perivascular Graft Repair
- routine forms of administration are insufficient
- to observe benefit given the heparin’s short half-life and complex pharmacokinetics.
- is complicated by the need for continuous infusion
- and the potential for uncontrolled hemorrhage.
- precisely regulate release kinetics,
- even site-specific therapy is prone to bleeding.
- poly(DL lactide-co-glycolide) (pLGA) microspheres sequestered in an alginate gel.
- gel permeation chromatography (GPC) and scanning electron microscopy (SEM)
- to monitor the degradation process and correlated well with the release kinetics.
- bovine vascular smooth muscle cells in a dose-dependent manner.
- and also controlled vascular injury in denuding and
- interposition vascular graft animal models of disease even when uncontrolled bleeding was evident with standard matrix-type release.
- the effects of various compounds in
- the control of smooth muscle cell proliferation in accelerated arteriopathies and also
- shed light on the biologic nature of these processes.(1)
- tissue surface chemistry and
- mechanical effects during organ function.
- high resistance to uniaxial or multiaxial loads
- dictated by a specific organ environment.
- aminated star polyethylene glycol and
- dextran aldehyde (PEG:dextran)
- under specific loading conditions, as well as
- tissue response at the adhesive material–tissue interface, can be modulated through regulation of
- the number and density of adhesive aldehyde groups.
- characterize the material aldehyde density available for tissue interaction,
- facilitating rapid, informed material choice.
Further, the correlation between AFM quantification of nanoscale unbinding forces
- with macroscale measurements of adhesion strength
- by uniaxial tension or multiaxial burst pressure allows the design of materials with specific cohesion and adhesion strengths.
- experiments are integrated along length scales to consider
- organ chemistry and mechanical loading states concurrently
- with adhesive material properties and tissue response. (2)
- responses to endothelial cell implants were investigated 3 months after angioplasty,
- approximately 2 months after the implants have degraded.
- reduced experimental restenosis compared to control by 56 and 31%, respectively.
- after 4 days in all animals implanted with xenogeneic cells.
- histologically at any of the implant sites at 90 days.
Suggesting that tissue engineered endothelial cell implants
- may provide long term control of vascular repair after injury,
- rather than simply delaying lesion formation and that
- allogeneic implants are able to provide a greater benefit than xenogeneic implants. (3)
- inhibit intimal thickening following acute balloon injury in pigs, and now seek to determine if these
- implants provide a similar benefit in the chronic and more complex injury model of arteriovenous anastomoses.
- toxicological,
- biological and
- immunological responses
were investigated 3 days and 1 and 2 months postoperatively to allogeneic endothelial cell implants . The anastomoses were wrapped with polymer matrices containing
- confluent porcine aortic endothelial cells (PAE; n = 14) or
- control matrices without cells (n = 10).
- compared to controls by 68% (p ! 0.05) at 2 months.
- differences in the rates of reendothelialization between the groups.
- are safe and reduce early intimal hyperplasia in a porcine model of arteriovenous anastomoses. (4)
onlinelibrary.wiley.com/doi/10.1002/anie.200461360/full
http://dx.doi.org/10.1016/j.actbio.2010.07.008.
Luminal Flow and Arterial Drug Delivery
- on arterial drug deposition after stent-based delivery is only now emerging.
- the influence of luminal flow patterns on arterial drug deposition and distribution.
- the coverage of tissue absorption of eluted drug and
- induce asymmetry in tissue drug distribution.
- sizes of the two recirculation zones and
- the asymmetry in drug distribution are determined by a complex interplay of local flow and strut geometry.
- pulsatile flow,
- the net luminal flow served as an index of flow-mediated spatiotemporal tissue drug uptake.
- luminal flow,
- strut design and
- pulsatility
- their respective therapeutic targets, FKBP12 and polymerized microtubules,
- while also associating in a more general manner with other tissue elements.
- locally released or systemically circulating drugs can
- displace DES drugs from their tissue binding domains.
- was assessed for both compounds simultaneously and
- in the presence of other commonly administered cardiac drugs.
- displace rapamycin and paclitaxel from general binding sites, possibly
- decreasing tissue reserve capacity for locally delivered drugs.
- to their biologically relevant specific protein targets, but
- can displace each other from tissue at three log order molar excess,
- decreasing arterial loads by greater than 50%.
- by stent design and
- stent deployment with custom-built stents.
- identical thin-strutted (81 m) devices in ex vivo flow loops (P< 0.001),
- 3 days after implantation in porcine coronary arteries (P 0.004).
- malapposed or overlapping configurations, thrombogenicity increased compared with apposed, length-matched controls (1.58-fold, P < 0.001; and 2.32-fold, P <0.001).
- lowest in all configurations and remained insensitive to incomplete deployment.
- predictions of stent-induced flow derangements
- correlated with spatial distribution of formed clots.
- they reduce thrombosis.
- are critical factors in modulating stent thrombogenicity.
- help reduce the potential for thrombosis
- despite complex stent configurations and variability in deployment. (Circulation. 2011;123:1400-1409.) (3)
Management of Obstructive Coronary Artery Disease
- efficacy of revascularization therapies and subsequent clinical outcomes.
- in the setting of multivessel coronary disease.
- revascularization with either PCI or CABG may be used.
- coronary artery bypass graft surgery provides better survival,
- fewer recurrent infarctions and
- greater freedom from re-intervention.
- that modulate drug distribution has hampered
- local pharmacotherapies in many organ systems.
- these are in part derived from transport forces,
- differences in deposition from tissue to tissue
This suggests that tissue ultrastructure also plays an important role.
- dextrans (a model hydrophilic drug similar to heparin) and albumin
- in orthogonal planes in arteries explanted from different vascular beds.
- geometric orientation and
- arterial connective tissue content.
- one to two orders of magnitude greater than across these sheaths.
- before decreasing for larger drugs.
- with almost 66% greater transfer into the thoracic aorta
- than into the carotid artery.
- dependent on arterial tissue content.
- in influencing vascular pharmacokinetics
- to potentially reduce restenosis in coronary arteries.
- is slowly released in the arterial wall to deliver a therapeutic dose to the target tissue.
- can contribute to the total radiation dose delivered to tissues.
- to model the transport of a hydrophilic drug released
- from the surface of a stent to the arterial media.
- near the stent struts giving rise to a
- non-uniform radiation activity distribution for the drug
- in the tissues as a function of time.
- resulting from this activity build-up in the arterial wall
- based on the medical internal radiation dose formalism.
- at the stent surface obtained from animal studies
- are used to normalize the results in terms of absolute dose to tissue.
- contributes only a small fraction of the total radiation delivered to the arterial wall,
- the main contribution comes from the activity embedded in the stent coating.
- the activity build-up in the arterial wall contributes only a small fraction
- to the total dose delivered by the P-32 ODN stent.
- would not improve the performance of radioactive stents in treating restenosis.
- makes accurate dosimetry difficult and
- the drug washout in the systemic circulatory system
- such as heparin have failed to stop restenosis clinically.
- differences in biology or differences in physicochemical properties and targeting.
- transport forces and device geometry on
- mean tissue concentration over a few micrometers.
- the ratio of convective to diffusive forces.
- they achieve higher mean concentrations and
- they remain closer to the intima.
- more negatively than hydrophobic drugs, and notably
- affect local concentrations without changing mean concentrations.
- these results provide a potential explanation for the variable success of stent-based delivery.
- does not ensure adequate targeting,
- because physiological transport forces cause
- local concentrations to deviate significantly from mean concentrations. (4)
- a spectrum of materials
- a range of manufacturing techniques, and have
- variable surfaces,
- dimensions,
- surface coverage, and
- strut configurations.
- flexibility,
- tracking ability,
- expansion,
- radiovisibility,
- side-branch access, and
- resistance to compression and recoil for different devices.
- toxicity,
- biocompatibility,
- structural and material analysis, and
- fatigue testing
- hoop strength,
- surface cracking,
- uniformity of expansion, and
- other features become standardized as well.
- minimal luminal diameter (MLD),
- percent diameter stenosis,
- late loss, or
- binary restenosis rate.
- the Palmaz-Schatz stent (Cordis-Johnson & Johnson).
- the variability between the Palmaz-Schatz stent groups in the different trials.
- complication rates rise as lesion complexity increases.
- ensure safety for all patients but are not the ideal venues in which to detect differences between devices.
Equivalency Trials
- not the means to evaluate the full potential of a device.
- patient entry and lesion selection be determined by
- limitations of the standard, not the device.
- the test device performs worse
- the average reference vessel size was 3.0+0.05 mm and
- American College of Cardiology type B2 and C lesions accounted for only ~65% of lesions.
- they represent only a minority of those lesions now receiving stents
Complexity, Equivalence, and Better
- thrombosis or restenosis and
- a continuous measure of indication,
- vessel dimension, or lesion complexity (Figure).
- differences in potential performance are anticipated.
- equivalency trials are limited to a small region of the curve.
- performed in lesions for which current devices have marginal or limited application.
- the next great challenges of interventional cardiology.
- the manner in which blood vessels are manipulated dictates biological sequelae.
- to change the way in which we consider design, approval, and use of new devices.
Menichelli, M. (2006). Sirolimus Stent vs. Bare Stent in Acute Myocardial Infarction Trial. Presented at The European Paris Course on Revascularization (EuroPCR), May 16-19, 2006, Paris, France Paris, France.http://www.medscape.com/viewprogram/5505?rss
Pfisterer, P.E. (2006). Basel Stent Cost-effectiveness Trial-Late Thrombotic events (BASKET LATE) Trial. Presented at American College of Cardiology 55th Annual Scientific Session, March 11 – 14, 2006, Atlanta, Georgia.http://www.medscape.com/viewprogram/5185
Rogers, C. Edelman E.R. (2006). Pushing drug-eluting stents into uncharted territory, Simpler then you think – more complex than you imagine. Circulation,113, 2262-2265.
Shirota, T., Yasui, H., Shimokawa, H. & Matsuda, T. (2003). Fabrication of endothelial progenitor cell (EPC)-seeded intravascular stent devices and in vitro endothelialization on hybrid vascular tissue. Biomaterials 24(13), 2295–2302.
Simonton, C. (2006). The STENT Registry: A real-world look at Sirolimus- and Pacitaxel-Eluting Stents. Cath Lab Digest, 14 (1), 1-10.
Turco, M. (2006). TAXUS ATLAS Trial – 9-Month results: Evaluation of TAXUS Liberte vs. TAXUS Express. Presented at The European Paris Course on Revascularization (EuroPCR), May 16-19, 2006, Paris, France Paris, France.http://www.medscape.com/viewprogram/5505?rss
Verma, S. and Marsden, P.A. (2005). Nitric Oxide-Eluting Polyurethanes – Vascular Grafts of the Future? New England Journal Medicine, 353 (7), 730-731.
Wood, S. (2006). Guidant suspends release of Xience V everolimus-eluting stent due to manufacturing standards http://www.theheart.org/article/679851.do
Other Related Articles that were published on this Open Access Online Scientific Journal include the following:
Larry H Bernstein, MD, FACP 3/2/2013
Quantum Biology And Computational Medicine
Larry H Bernstein, MD, FACP 4/3/2013
Virtual Biopsy – is it possible?
Larry H Bernstein, MD, FACP 3/3/2013
Reprogramming cell fate 3/2/2013
Larry H Bernstein, MD, FACP
How Methionine Imbalance with Sulfur-Insufficiency Leads to Hyperhomocysteinemia
Larry H Bernstein, MD, FACP 4/4/2013
http://pharmaceuticalintelligence.com/2013/04/04/sulfur-deficiency-and-hyperhomocusteinemia/
Amyloidosis with Cardiomyopathy
Larry H Bernstein, MD, FACP 3/31/2013
http://pharmaceuticalintelligence.com/2013/03/31/amyloidosis-with-cardiomyopathy/
Nitric Oxide, Platelets, Endothelium and Hemostasis
Larry H Bernstein, MD, FACP 11/8/2012
http://pharmaceuticalintelligence.com/2012/11/08/nitric-oxide-platelets-endothelium-and-hemostasis/
Mitochondrial Damage and Repair under Oxidative Stress
Larry H Bernstein, MD, FACP 10/28/2012
Endothelial Function and Cardiovascular Disease
Larry H Bernstein, MD, FACP 10/25/2012
http://pharmaceuticalintelligence.com/2012/10/25/endothelial-function-and-cardiovascular-disease/
Aviva Lev-Ari, PhD, RN 8/27/2012
Revascularization: PCI, Prior History of PCI vs CABG
Aviva Lev-Ari, PhD, RN 4/25/2013
http://pharmaceuticalintelligence.com/2013/04/25/revascularization-pci-prior-history-of-pci-vs-cabg/
Cholesteryl Ester Transfer Protein (CETP) Inhibitor: Potential of Anacetrapib to treat Atherosclerosis and CAD
Aviva Lev-Ari, PhD, RN 4/7/2013
Hypertriglyceridemia concurrent Hyperlipidemia: Vertical Density Gradient Ultracentrifugation a Better Test to Prevent Undertreatment of High-Risk Cardiac Patients
Aviva Lev-Ari, PhD, RN 4/4/2013
Fight against Atherosclerotic Cardiovascular Disease: A Biologics not a Small Molecule – Recombinant Human lecithin-cholesterol acyltransferase (rhLCAT) attracted AstraZeneca to acquire AlphaCore
Aviva Lev-Ari, PhD, RN 4/3/2013
High-Density Lipoprotein (HDL): An Independent Predictor of Endothelial Function & Atherosclerosis, A Modulator, An Agonist, A Biomarker for Cardiovascular Risk
Aviva Lev-Ari, PhD, RN 3/31/2013
Acute Chest Pain/ER Admission: Three Emerging Alternatives to Angiography and PCI
Aviva Lev-Ari, PhD, RN 3/10/2013
Genomics & Genetics of Cardiovascular Disease Diagnoses: A Literature Survey of AHA’s Circulation Cardiovascular Genetics, 3/2010 – 3/2013
Lev-Ari, A. and L H Bernstein 3/7/2013
The Heart: Vasculature Protection – A Concept-based Pharmacological Therapy including THYMOSIN
Aviva Lev-Ari, PhD, RN 2/28/2013
Arteriogenesis and Cardiac Repair: Two Biomaterials – Injectable Thymosin beta4 and Myocardial Matrix Hydrogel
Aviva Lev-Ari, PhD, RN 2/27/2013
Coronary artery disease in symptomatic patients referred for coronary angiography: Predicted by Serum Protein Profiles
Aviva Lev-Ari, PhD, RN 12/29/2012
Special Considerations in Blood Lipoproteins, Viscosity, Assessment and Treatment
Bernstein, HL and Lev-Ari, A. 11/28/2012
Peroxisome proliferator-activated receptor (PPAR-gamma) Receptors Activation: PPARγ transrepression for Angiogenesis in Cardiovascular Disease and PPARγ transactivation for Treatment of Diabetes
Aviva Lev-Ari, PhD, RN 11/13/2012
Clinical Trials Results for Endothelin System: Pathophysiological role in Chronic Heart Failure, Acute Coronary Syndromes and MI – Marker of Disease Severity or Genetic Determination?
Aviva Lev-Ari, PhD, RN 10/19/2012
Endothelin Receptors in Cardiovascular Diseases: The Role of eNOS Stimulation
Aviva Lev-Ari, PhD, RN 10/4/2012
Inhibition of ET-1, ETA and ETA-ETB, Induction of NO production, stimulation of eNOS and Treatment Regime with PPAR-gamma agonists (TZD): cEPCs Endogenous Augmentation for Cardiovascular Risk Reduction – A Bibliography
Aviva Lev-Ari, PhD, RN 10/4/2012
Positioning a Therapeutic Concept for Endogenous Augmentation of cEPCs — Therapeutic Indications for Macrovascular Disease: Coronary, Cerebrovascular and Peripheral
Aviva Lev-Ari, PhD, RN 8/29/2012
Cardiovascular Outcomes: Function of circulating Endothelial Progenitor Cells (cEPCs): Exploring Pharmaco-therapy targeted at Endogenous Augmentation of cEPCs
Aviva Lev-Ari, PhD, RN 8/28/2012
Endothelial Dysfunction, Diminished Availability of cEPCs, Increasing CVD Risk for Macrovascular Disease – Therapeutic Potential of cEPCs
Aviva Lev-Ari, PhD, R N 8/27/2012
Vascular Medicine and Biology: CLASSIFICATION OF FAST ACTING THERAPY FOR PATIENTS AT HIGH RISK FOR MACROVASCULAR EVENTS Macrovascular Disease – Therapeutic Potential of cEPCs
Aviva Lev-Ari, PhD, RN 8/24/2012
Cardiovascular Disease (CVD) and the Role of agent alternatives in endothelial Nitric Oxide Synthase (eNOS) Activation and Nitric Oxide Production
Aviva Lev-Ari, PhD, RN 7/19/2012
Resident-cell-based Therapy in Human Ischaemic Heart Disease: Evolution in the PROMISE of Thymosin beta4 for Cardiac Repair
Aviva Lev-Ari, PhD, RN 4/30/2012
http://pharmaceuticalintelligence.com/2012/04/30/93/
Triple Antihypertensive Combination Therapy Significantly Lowers Blood Pressure in Hard-to-Treat Patients with Hypertension and Diabetes
Aviva Lev-Ari, PhD, RN 5/29/2012
http://pharmaceuticalintelligence.com/2012/05/29/445/
Macrovascular Disease – Therapeutic Potential of cEPCs: Reduction Methods for CV Risk
Aviva Lev-Ari, PhD, RN 7/2/2012
Mitochondria Dysfunction and Cardiovascular Disease – Mitochondria: More than just the “powerhouse of the cell”
Aviva Lev-Ari, PhD, RN 7/9/2012
Bystolic’s generic Nebivolol – positive effect on circulating Endothelial Proginetor Cells endogenous augmentation
Aviva Lev-Ari, PhD, RN 7/16/2012
Arteriogenesis and Cardiac Repair: Two Biomaterials – Injectable Thymosin beta4 and Myocardial Matrix Hydrogel
Aviva Lev-Ari, PhD, RN 2/27/2013
Cardiac Surgery Theatre in China vs. in the US: Cardiac Repair Procedures, Medical Devices in Use, Technology in Hospitals, Surgeons’ Training and Cardiac Disease Severity”
Aviva Lev-Ari, PhD, RN 1/8/2013
Heart Remodeling by Design – Implantable Synchronized Cardiac Assist Device: Abiomed’s Symphony
Aviva Lev-Ari, PhD, RN 7/23/2012
Acute Chest Pain/ER Admission: Three Emerging Alternatives to Angiography and PCI
Aviva Lev-Ari, PhD, RN 3/10/2013
Dilated Cardiomyopathy: Decisions on implantable cardioverter-defibrillators (ICDs) using left ventricular ejection fraction (LVEF) and Midwall Fibrosis: Decisions on Replacement using late gadolinium enhancement cardiovascular MR (LGE-CMR)
Aviva Lev-Ari, PhD, RN 3/10/2013
http://pharmaceuticalintelligence.com/2013/03/10/dilated-cardiomyopathy-decisions-on-implantable-cardioverter-defibrillators-icds-using-left-ventricular-ejection-fraction-lvef-and-midwall-fibrosis-decisions-on-replacement-using-late-gadolinium/
The Heart: Vasculature Protection – A Concept-based Pharmacological Therapy including THYMOSIN
Aviva Lev-Ari, PhD, RN 2/28/2013
http://pharmaceuticalintelligence.com/2013/02/28/the-heart-vasculature-protection-a-concept-based-pharmacological-therapy-including-thymosin/
FDA Pending 510(k) for The Latest Cardiovascular Imaging Technology
Aviva Lev-Ari, PhD, RN 1/28/2013
http://pharmaceuticalintelligence.com/2013/01/28/fda-pending-510k-for-the-latest-cardiovascular-imaging-technology/
PCI Outcomes, Increased Ischemic Risk associated with Elevated Plasma Fibrinogen not Platelet Reactivity
Aviva Lev-Ari, PhD, RN 1/10/2013
http://pharmaceuticalintelligence.com/2013/01/10/pci-outcomes-increased-ischemic-risk-associated-with-elevated-plasma-fibrinogen-not-platelet-reactivity/
The ACUITY-PCI score: Will it Replace Four Established Risk Scores — TIMI, GRACE, SYNTAX, and Clinical SYNTAX
Aviva Lev-Ari, PhD, RN
http://pharmaceuticalintelligence.com/2013/01/03/the-acuity-pci-score-will-it-replace-four-established-risk-scores-timi-grace-syntax-and-clinical-syntax/
Coronary artery disease in symptomatic patients referred for coronary angiography: Predicted by Serum Protein Profiles
Aviva Lev-Ari, PhD, RN
http://pharmaceuticalintelligence.com/2012/12/29/coronary-artery-disease-in-symptomatic-patients-referred-for-coronary-angiography-predicted-by-serum-protein-profiles/
Heart Renewal by pre-existing Cardiomyocytes: Source of New Heart Cell Growth Discovered
Aviva Lev-Ari, PhD, RN 12/23/2012
http://pharmaceuticalintelligence.com/2012/12/23/heart-renewal-by-pre-existing-cardiomyocytes-source-of-new-heart-cell-growth-discovered/
Cardiovascular Risk Inflammatory Marker: Risk Assessment for Coronary Heart Disease and Ischemic Stroke – Atherosclerosis.
Aviva Lev-Ari, PhD, RN 10/30/2012
http://pharmaceuticalintelligence.com/2012/10/30/cardiovascular-risk-inflammatory-marker-risk-assessment-for-coronary-heart-disease-and-ischemic-stroke-atherosclerosis/
To Stent or Not? A Critical Decision
Aviva Lev-Ari, PhD, RN 10/23/2012
http://pharmaceuticalintelligence.com/2012/10/23/to-stent-or-not-a-critical-decision/
New Definition of MI Unveiled, Fractional Flow Reserve (FFR)CT for Tagging Ischemia
Aviva Lev-Ari, PhD, RN 8/27/2012
http://pharmaceuticalintelligence.com/2012/08/27/new-definition-of-mi-unveiled-fractional-flow-reserve-ffrct-for-tagging-ischemia/
Ethical Considerations in Studying Drug Safety — The Institute of Medicine Report
Aviva Lev-Ari, PhD, RN 8/23/2012
http://pharmaceuticalintelligence.com/2012/08/23/ethical-considerations-in-studying-drug-safety-the-institute-of-medicine-report/
New Drug-Eluting Stent Works Well in STEMI
Aviva Lev-Ari, PhD, RN 8/22/2012
http://pharmaceuticalintelligence.com/2012/08/22/new-drug-eluting-stent-works-well-in-stemi/
Expected New Trends in Cardiology and Cardiovascular Medical Devices
Aviva Lev-Ari, PhD, RN 8/17/2012
http://pharmaceuticalintelligence.com/2012/08/17/expected-new-trends-in-cardiology-and-cardiovascular-medical-devices/
Coronary Artery Disease – Medical Devices Solutions: From First-In-Man Stent Implantation, via Medical Ethical Dilemmas to Drug Eluting Stents
Aviva Lev-Ari, PhD, RN 8/13/2012
Percutaneous Endocardial Ablation of Scar-Related Ventricular Tachycardia
Aviva Lev-Ari, PhD, RN 7/18/2012
Competition in the Ecosystem of Medical Devices in Cardiac and Vascular Repair: Heart Valves, Stents, Catheterization Tools and Kits for Open Heart and Minimally Invasive Surgery (MIS)
Aviva Lev-Ari, PhD, RN 6/22/2012
Global Supplier Strategy for Market Penetration & Partnership Options (Niche Suppliers vs. National Leaders) in the Massachusetts Cardiology & Vascular Surgery Tools and Devices Market for Cardiac Operating Rooms and Angioplasty Suites
Aviva Lev-Ari, PhD, RN 6/22/2012
- Contributions to vascular biology – Elazer Edelman Lab (pharmaceuticalintelligence.com)
- Irish-made next-generation coronary stent system implanted in Dublin (siliconrepublic.com)
- UF&Shands One Of First Facilities Approved To Use Drug-Coated Stent For Peripheral Artery Disease (medicalnewstoday.com)
- Data Published in JACC: Cardiovascular Interventions Show that OrbusNeich’s COMBO Dual Therapy Stent™ Reaches Primary Study Endpoint and Is Effective in Controlling Neointimal Proliferation (sys-con.com)
- How does a Coronary Stent Work? (healthdisturbances.com)
- North America Leads Drug Delivery Technologies Market Followed by Europe Says New Research Report at ReportsnReports.com (prweb.com)
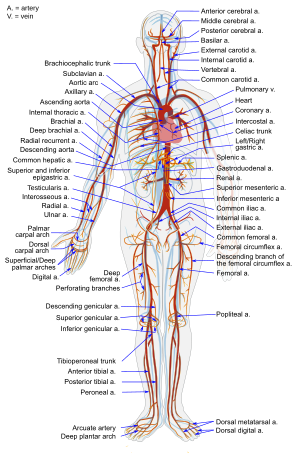
English: simplified diagram of the human Arterial system in anterior view. Français : Diagramme simplifié du système artériel humain en vue antérieure (en anglais). (Photo credit: Wikipedia)

