Statins’ Nonlipid Effects on Vascular Endothelium through eNOS Activation
Curator, Author,Writer, Reporter: Larry Bernstein, MD, FACP
Categories of Research:
Disease biology, Cell Biology and Cell Signaling, Biological Networks and Gene Regulation, Pharmacotherapy of Cardiovascular Disease, Nitric Oxide, HMG Co A inhibitors, Endothelial Receptor, Hypertension, Therapeutic Targets
Introduction
Statins have an effect on the vascular endothelium, which plays an important role in the development of atherosclerosis and angiogenesis, a role independent of the lipid lowering effect. The vascular endothelium plays an important role regulating vascular wall contraction and as a mediator for the vascular wall. Endothelial dysfunction, the hallmark of which is reduced activity of endothelial cell derived nitric oxide (NO), is a key factor in developing atherosclerosis and cardiovascular disease. Vascular endothelial cells play a pivotal role in modulation of leukocyte and platelet adherence, thrombogenicity, anticoagulation, and vessel wall contraction and relaxation, so that endothelial dysfunction has become almost a synonym for vascular disease. A single layer of endothelial cells is the only constituent of capillaries, which differ from other vessels, which contain smooth muscle cells and adventitia. Capillaries directly mediate nutritional supply as well as gas exchange within all organs. The failure of the microcirculation leads to tissue apoptosis/necrosis. expanded cultured EPC transplantation and cytokine-induced EPC mobilization from bone marrow have been shown to enhance angiogenesis with significant improvement of microcirculation in ischemic tissue.
It has been generally assumed that cholesterol reduction by statins mechanism underlying their beneficial effects in cardiovascular disease. The statins — potent inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, an enzyme that plays a critical role in cholesterol metabolism — block substrate accessibility to HMG-CoA reductase , effectively subverting cholesterol metabolism. Sufficient evidence now supports a hypothesis that cholesterol-independent or “pleiotropic” effects of statins improve endothelial dysfunction, effects on angiogenesis, and reduce vascular inflammation. The statins’ cholesterol-independent vascular effects appear to directly restore or improve endothelial function by increasing NO production, promote endothelial repair after arterial injury, and decrease vascular inflammation. Statins improve endothelial function by:
- increasing production of nitric oxide,
- promoting blood flow,
- dampening inflammation,
- antagonizing thrombogenicity, and
- reducing endothelial vasoresponses.
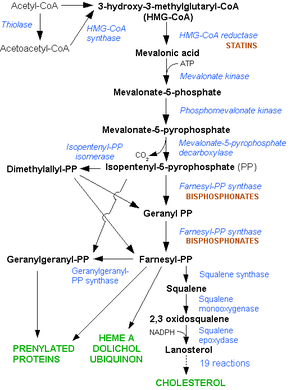
The HMG-CoA reductase pathway, which is blocked by statins via inhibiting the rate limiting enzyme HMG-CoA reductase. (Photo credit: Wikipedia)
We review effects of statins on endothelial cells and endothelial progenitor cells that identifies a novel therapeutic potential of statin drugs.
- Evidence in support of the new “pleiotrophic” non-lipid effects of Statins
- Endothelial cell progenitors leave the bone marrow in response to cytokines or ischemic Injury.
- They proliferate, migrate, and acquire resistance to apoptotic cell death.
Transplanting mice with the bone marrow of a transgenic animal carrying the LacZ reporter gene under control of the Tie2 promoter, which is active in endothelial cells…showed that statin-treated animals accumulate marrow-derived endothelial cells at the site of corneal neovascularization, administering statins is probably safer than giving VEGF to promote angiogenesis or vasculogenesis.
- Akt activation has emerged as an indispensable signaling gateway at the crossroads between angiogenesis and endothelial stem cell recruitment and differentiation
- Placental growth factor, which seems preferentially involved in facilitating postnatal blood vessel formation, is another “vasculogenic factor” that acts very much like the statins
- Increase in endothelial nitric oxide synthase expression and activity is clearly stimulated by statins, which results in Akt activation a multifaceted developmental pathway of stem cell mobilization and differentiation is exploited by statins
Altieri DC. Statins’ benefits begin to sprout. J. Clin. Invest. 108:365–366 (2001). DOI:10.1172/JCI200113556
“Pleiotropic” Effect of statins
Recent studies have shown the restoration of endothelial function before significant reduction of serum cholesterol levels effect of statins on the endothelium were first defined by their ability to enhance endothelial NO production, upregulating endothelial nitric oxide synthase (eNOS) PI3 kinase/Akt signaling, which is a crucial regulator of cell metabolism and apoptosis, appears to mediate statin-induced eNOS upregulation.
The mechanism of eNOS activation by phosphorylation by statins
Statins can also inhibit Rho isoprenylation/activation resulting in enhanced eNOS mRNA stability and increased eNOS expression statins inhibit ox-LDL-induced endothelin-1 (ET-1) expression and the biological function of angiotensin II, and its receptor subtype 1 (AT1), which are both potent vasoconstrictors/mitogens thought to contribute to the development of atherosclerotic lesions.
Vascular inflammation
Statins have been shown to reduce the number of inflammatory cells in atherosclerotic lesions. Inhibitory effects of statins on adhesion molecules such as intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule (VCAM-1) and E-selectin, which are involved in the adhesion/rolling/extravasation of inflammatory cells.
Statin therapy in humans has also been shown to lower high-sensitivity C-Reactive Protein (hs-CRP), which reflects low-grade systemic/vascular inflammation, in hypercholesterolemic patients. This has been shown to correlate with reductions in the rates of acute major or recurrent coronary events.
Re-endothelialization
Accelerated re-endothelialization after angioplasty/de-endothelialization is known to inhibit neointimal hyperplasia, which leads to luminal narrowing or restenosis at the injured site. Re-endothelialization has been shown to be promoted by vascular endothelial growth factor (VEGF), hepatocyte growth factor (HGF), estrogen, prostacyclin, blockade of TNFα, and now Statins.
Ii M, Losordo DW. Statins and the endothelium. Vascular Pharmacology 2007; 46: 1–9.
Altieri DC. Statins’ benefits begin to sprout. J. Clin. Invest. 108:365–366 (2001). DOI:10.1172/JCI200113556
Further observations
- Statins exert cholesterol-independent effects on the endothelium, which lead to the improvement of endothelial function.
- Statins exert biphasic, dose dependent effects on angiogenesis. At low doses, statins induce angiogenesis, whereas angiogenesis is inhibited at higher doses. These biphasic activities of statins on endothelial cell biology can be explained by the properties of the biosynthetic pathways that originate from mevalonic acid.
- It appears that low concentrations of statins (such as those achieved in vivo) induce pro-angiogenic effects through activating PI3 kinase/Akt signaling leading to eNOS phosphorylation and NO production.
- High (supra-physiologic) concentrations of statins will inhibit the synthesis of the non-sterol products mevalonate, leading to decreases in protein prenylation, inhibition of cell growth, or apoptosis.
The sum-up of two factors: the loss of the vascular relaxation directly dependent of the endothelium (flow – dependent) and the NO dependent are the main reason for endothelial dysfunction and play a very important role in the pathogenesis of heart failure.
- Endothelial dysfunction on vascular peripheral levels contributes to the increased peripheral resistance in patients with heart failure. Endothelial dysfunction, as a pathophysiology disorder, is present early.
- Statins’ benefits begin to sprout in the initiation of the atherosclerotic process.
- The injury of eNOS activity seems to occur with impaired coronary vasodilatation in response to acetylcholine in patients with hypertension, hypercholesterolemia, diabetes, smokers.
Summary of Key Points
Mechanisms which are essential for the impairment of eNOS activity for the appearance of endothelial dysfunction are:
• dysfunctional signal transduction receptor – endothelial cell;
• decreased bioavailability of the substrate L- arginine;
• altered expression of gene NOS3 and stability of mARN; polymorphism NOS3;
• altered eNOS activity;
• increased destruction of NO;
• changes in the balance between NO derived endothelium and the hyperpolarizing factor (EDHF);
• decreased sensitivity of atherosclerotic smooth muscle to NO.
Effects other than those due to lowering LDL levels and independent of the LDL level
• improved endothelial function
• diminish vascular inflammation
• improve ventricular function of heart failure
• antithrombotic effect
• reduce the rate of vascular events
• antioxidant effect
Statins improve endothelial function through the following mechanisms:
• enhanced endothelial NO production by decrease of cholesterol, by up regulating posttranscriptional mRNA of eNOS and by antioxidative effects (reduction of reactive oxygen species, increase of super oxide elimination and decrease of oxidized LDL);
• reduced production of endothelin-1, endothelial vasoconstrictor factor;
• diminish the affinity for AT1 receptors ;
• stimulation of angiogenesis through proliferation, migration and survival of the circulating endothelial progenitor cells
Statins decrease the swell of the vascular wall by:
• decreasing the level of C – Reactive Protein
• decreasing the synthesis of proinflammatory cytokines (IL-1, IL-6, IL-8, TNF α)
• diminishing the leukocyte adhesion to endothelial cells inhibiting macrophage growth and smooth muscle cell migration and proliferation
Suciu M. The Role Of Nitric Oxide (No) And Statins In Endothelial Dysfunction And Atherosclerosis. Farmacia 2009; 57 (2): 131-139
Relevant observations
ECs treated with rosuvastatin increase eNOS activation. The increased NO production is involved in modulating S-nitrosylation and translation of proteins.
Bin Huang, Fu An Li, Chien Hsing Wu, Danny Ling Wang. The role of nitric oxide on rosuvastatin-mediated S-nitrosylation and translational proteomes in human umbilical vein endothelial cells. Proteome Science 2012, 10:43. doi:10.1186/1477-5956-10-43
Emerging evidence from both clinical trials and basic science studies suggest that statins have anti-inflammatory properties, which may additionally lead to clinical efficacy. Measurement of markers of inflammation such as high sensitivity C-Reactive Protein in addition to lipid parameters may help identify those patients who will benefit most from statin therapy.
Blake GJ and Ridker PM. Are statins anti-inflammatory? Curr Control Trials Cardiovasc Med 2000, 1:161–165.
Most favorable and unexpected findings were:
- new indications for TDZs as stimulators of eNOS, in addition to the new indication for atherosclerosis besides the classic indication in pharmacology books, being in the reduction of insulin resistance.
- new indications for beta blockers as NO stimulant, nebivolol, a case in point, thus, fulfilling two indications in one drug along the direction of the study to identify eNOS agonists. Nebivolol is a vasodilator, thus functions as an antihypertensive.
Aviva Lev-Ari. Cardiovascular Disease (CVD) and the Role of agent alternatives in endothelial Nitric Oxide Synthase (eNOS) Activation and Nitric Oxide Production. July 19, 2012 pharmaceuticalintelligence.com
References
Heeba G, Hassan MK, Khalifa, M; Malinski T. Adverse Balance of Nitric Oxide/ Peroxynitrite in the Dysfunctional Endothelium Can be Reversed by Statins. Journal of Cardiovascular Pharmacology. 2007; 50(4):391-398.
Tandon VR, Gupta BM, Tandon R. Non-lipid Actions of Statins. JK Science 2004; 6(3): 124-126.
Sacks FM. Do statins play a role in the early management of the acute coronary syndrome? European Heart Journal Supplements (2004) 6 (Supplement A), A32–A36.
Alonso D, Radomski MW. Nitric oxide, platelet function, myocardial infarction and reperfusion therapies. Heart Fail Rev 2003; 8:47–54.
Cardiovascular Disease (CVD) and the Role of agent alternatives in endothelial Nitric Oxide Synthase (eNOS) Activation and Nitric Oxide Production. PharmaceuticalIntelligence.WordPress.com
Nitric oxide and signalling pathways. PharmaceuticalIntelligence.WordPress.com
Rationale of NO use in hypertension and heart failure. PharmaceuticalIntelligence.WordPress.com
LH Bernstein. Mitochondria: Origin from oxygen free environment, role in aerobic glycolysis, metabolic adaptation in cancer (Warburg effect). PharmaIntell.Wordpress.com
R Saxena. Mitochondria: More than just the powerhouse of the cell. PharmaIntell.WordPress.com
Bernstein LH. Expanding the Genetic Alphabet and linking the genome to the metabolome. PharmaIntell.wordpress.com. luly 24, 2012.
R saxena. β Integrin emerges as an important player in mitochondrial dysfunction associated Gastric Cancer. PharmaIntell.wordpress.com 2012
Related articles
- Interaction of Nitric Oxide and Prostacyclin in Vascular Endothelium (pharmaceuticalintelligence.com)
- Angiogenesis Impairment in Diabetes: Role of Methylglyoxal-Induced Receptor for Advanced Glycation Endproducts, Autophagy and Vascular Endothelial Growth Factor Receptor 2 (plosone.org)
- Endothelial Dysfunction, Diminished Availability of cEPCs, Increasing CVD Risk for Macrovascular Disease – Therapeutic Potential of cEPCs (pharmaceuticalintelligence.com)
- Inhibition of Proliferation, Migration and Proteolysis Contribute to Corticosterone-Mediated Inhibition of Angiogenesis (plosone.org)
- Nitric Oxide has a ubiquitous role in the regulation of glycolysis -with a concomitant influence on mitochondrial function (pharmaceuticalintelligence.com)
- Nitric Oxide Covalent Modifications: A Putative Therapeutic Target? (pharmaceuticalintelligence.com)
- Discovery of nitric oxide and its role in vascular biology (pharmaceuticalintelligence.com)