Brain Biobank and studies of disease structure correlates
Larry H. Bernstein, MD, FCAP, Curator
LPBI

The research team, led by Isaac Kohane at HMS and Roy Perlis at Mass General, has created a neuropsychiatric cellular biobank—one of the largest in the world.
It contains induced pluripotent stem cells, or iPSCs, derived from skin cells taken from 100 people with neuropsychiatric diseases such as schizophrenia, bipolar disorder and major depression, and from 50 people without neuropsychiatric illness.
In addition, a detailed profile of each patient, obtained from hours of in-person assessment as well as from electronic medical records, is matched to each cell sample.
As a result, the scientific community can now for the first time access cells representing a broad swath of neuropsychiatric illness. This enables researchers to correlate molecular data with clinical information in areas such as variability of drug reactions between patients. The ultimate goal is to help treat, with greater precision, conditions that often elude effective management.
The cell collection and generation was led by investigators at Mass General, who in collaboration with Kohane and his team are working to characterize the cell lines at a molecular level. The cell repository, funded by the National Institutes of Health, is housed at Rutgers University.
“This biobank, in its current form, is only the beginning,” said Perlis, director of the MGH Psychiatry Center for Experimental Drugs and Diagnostics and HMS associate professor of psychiatry. “By next year we’ll have cells from a total of four hundred patients, with additional clinical detail and additional cell types that we will share with investigators.”
A current major limitation to understanding brain diseases is the inability to access brain biopsies on living patients. As a result, researchers typically study blood cells from patients or examine post-mortem tissue. This is in stark contrast with diseases such as cancer, for which there are many existing repositories of highly characterized cells from patients.
The new biobank offers a way to push beyond this limitation.
A Big Step Forward
While the biobank is already a boon to the scientific community, researchers at MGH and the HMS Department of Biomedical Informatics will be adding additional layers of molecular data to all of the cell samples. This information will include whole genome sequencing and transcriptomic and epigenetic profiling of brain cells made from the stem cell lines.
Collaborators in the HMS Department of Neurobiology, led by Michael Greenberg, department chair and Nathan Marsh Pusey Professor of Neurobiology, will also work to examine characteristics of other types of neurons derived from these stem cells.
“This can potentially alter the entire way we look at and diagnose many neuropsychiatric conditions,” said Perlis.
One example may be to understand how the cellular responses to medication correspond to the patient’s documented responses, comparing in vitro with in vivo. “This would be a big step forward in bringing precision medicine to psychiatry,” Perlis said.
“It’s important to recall that in the field of genomics, we didn’t find interesting connections to disease until we had large enough samples to really investigate these complex conditions,” said Kohane, chair of the HMS Department of Biomedical Informatics.
“Our hypothesis is that here we will require far fewer patients,” he said. “By measuring the molecular functioning of the cells of each patient rather than only their genetic risk, and combining that all that’s known of these people in terms of treatment response and cognitive function, we will discover a great deal of valuable information about these conditions.”
Added Perlis, “In the early days of genetics, there were frequent false positives because we were studying so few people. We’re hoping to avoid the same problem in making cellular models, by ensuring that we have a sufficient number of cell lines to be confident in reporting differences between patient groups.”
The generation of stem cell lines and characterization of patients and brain cell lines is funded jointly by the the National Institute of Mental Health, the National Human Genome Research Institute and a grant from the Centers of Excellence in Genomic Science program.
On C.T.E. and Athletes, Science Remains in Its Infancy
Se Hoon Choi, Young Hye Kim, Matthias Hebisch, et al.
http://www.nature.com/articles/nature13800.epdf
Alzheimer’s disease is the most common form of dementia, characterized by two pathological hallmarks: amyloid-β plaques and neurofibrillary tangles1. The amyloid hypothesis of Alzheimer’s disease posits that the excessive accumulation of amyloid-β peptide leads to neurofibrillary tangles composed of aggregated hyperphosphorylated tau2, 3. However, to date, no single disease model has serially linked these two pathological events using human neuronal cells. Mouse models with familial Alzheimer’s disease (FAD) mutations exhibit amyloid-β-induced synaptic and memory deficits but they do not fully recapitulate other key pathological events of Alzheimer’s disease, including distinct neurofibrillary tangle pathology4, 5. Human neurons derived from Alzheimer’s disease patients have shown elevated levels of toxic amyloid-β species and phosphorylated tau but did not demonstrate amyloid-β plaques or neurofibrillary tangles6, 7, 8, 9, 10, 11. Here we report that FAD mutations in β-amyloid precursor protein and presenilin 1 are able to induce robust extracellular deposition of amyloid-β, including amyloid-β plaques, in a human neural stem-cell-derived three-dimensional (3D) culture system. More importantly, the 3D-differentiated neuronal cells expressing FAD mutations exhibited high levels of detergent-resistant, silver-positive aggregates of phosphorylated tau in the soma and neurites, as well as filamentous tau, as detected by immunoelectron microscopy. Inhibition of amyloid-β generation with β- or γ-secretase inhibitors not only decreased amyloid-β pathology, but also attenuated tauopathy. We also found that glycogen synthase kinase 3 (GSK3) regulated amyloid-β-mediated tau phosphorylation. We have successfully recapitulated amyloid-β and tau pathology in a single 3D human neural cell culture system. Our unique strategy for recapitulating Alzheimer’s disease pathology in a 3D neural cell culture model should also serve to facilitate the development of more precise human neural cell models of other neurodegenerative disorders.
Figure 2: Robust increases of extracellular amyloid-β deposits in 3D-differentiated hNPCs with FAD mutations.close
![Robust increases of extracellular amyloid-[bgr] deposits in 3D-differentiated hNPCs with FAD mutations.](https://i0.wp.com/www.nature.com/nature/journal/v515/n7526/carousel/nature13800-f2.jpg?resize=121%2C200)
a, Thin-layer 3D culture protocol. HC, histochemistry; IF, immunofluorescence; IHC, immunohistochemistry. b, Amyloid-β deposits in 6-week differentiated control and FAD ReN cells in 3D Matrigel (green, GFP; blue, 3D6; scale bar, …
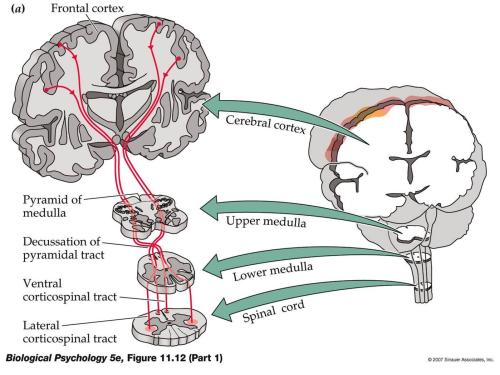
Stem Cell-Based Spinal Cord Repair Enables Robust Corticospinal Regeneration
Novel use of EPR spectroscopy to study in vivo protein structure
α-synuclein
α-synuclein is a protein found abundantly throughout the brain. It is present mainly at the neuron ends where it is thought to play a role in ensuring the supply of synaptic vesicles in presynaptic terminals, which are required for the release of neurotransmitters to relay signals between neurons. It is critical for normal brain function.
However, α-synuclein is also the primary protein component of the cerebral amyloid deposits characteristic of Parkinson’s disease and its precursor is found in the amyloid plaques of Alzheimer’s disease. Although α-synuclein is present in all areas of the brain, these disease-state amyloid plaques only arise in distinct areas.

Alpha-synuclein protein. May play role in Parkinson’s and Alzheimer’s disease. © molekuul.be / Shutterstock.com
Imaging of isolated samples of α-synuclein in vitro indicate that it does not have the precise 3D folded structure usually associated with proteins. It is therefore classed as an intrinsically disordered protein. However, it was not known whether the protein also lacked a precise structure in vivo.
There have been reports that it can form helical tetramers. Since the 3D structure of a biological protein is usually precisely matched to the specific function it performs, knowing the structure of α-synuclein within a living cell will help elucidate its role and may also improve understanding of the disease states with which it is associated.
If α-synuclein remains disordered in vivo, it may be possible for the protein to achieve different structures, and have different properties, depending on its surroundings.
Techniques for determining protein structure
It has long been known that elucidating the structure of a protein at an atomic level is fundamental for understanding its normal function and behavior. Furthermore, such knowledge can also facilitate the development of targeted drug treatments. Unfortunately, observing the atomic structure of a protein in vivo is not straightforward.
X-ray diffraction is the technique usually adopted for visualizing structures at atomic resolution, but this requires crystals of the molecule to be produced and this cannot be done without separating the molecules of interest from their natural environment. Such processes can modify the protein from its usual state and, particularly with complex structures, such effects are difficult to predict.
The development of nuclear magnetic resonance (NMR) spectroscopy improved the situation by making it possible for molecules to be analyzed under in vivo conditions, i.e. same pH, temperature and ionic concentration.
More recently, increases in the sensitivity of NMR and the use of isotope labelling have enabled determinations of the atomic level structure and dynamics of proteins to be determined within living cells1. NMR has been used to determine the structure of a bacterial protein within living cells2 but it is difficult to achieve sufficient quantities of the required protein within mammalian cells and to keep the cells alive for NMR imaging to be conducted.
Electron paramagnetic resonance (EPR) spectroscopy for determining protein structure
Recently, researchers have managed to overcome these obstacles by using in-cell NMR and electron paramagnetic resonance (EPR) spectroscopy. EPR spectroscopy is a technique that is similar to NMR spectroscopy in that it is based on the measurement and interpretation of the energy differences between excited and relaxed molecular states.
In EPR spectroscopy it is electrons that are excited, whereas in NMR signals are created through the spinning of atomic nuclei. EPR was developed to measure radicals and metal complexes, but has also been utilized to study the dynamic organization of lipids in biological membranes3.
EPR has now been used for the first time in protein structure investigations and has provided atomic-resolution information on the structure of α-synuclein in living mammalians4,5.
Bacterial forms of the α-synuclein protein labelled with 15N isotopes were introduced into five types of mammalian cell using electroporation. Concentrations of α-synuclein close to those found in vivo were achieved and the 15N isotopes allowed the protein to be clearly defined from other cellular components by NMR. The conformation of the protein was then determined using electron paramagnetic resonance (EPR).
The results showed that within living mammalian cells α-synuclein remains as a disordered and highly dynamic monomer. Different intracellular environments did not induce major conformational changes.
Summary
The novel use of EPR spectroscopy has resolved the mystery surrounding the in vivo conformation of α-synuclein. It showed that α-synuclein maintains its disordered monomeric form under physiological cell conditions. It has been demonstrated for the first time that even in crowded intracellular environments α-synuclein does not form oligomers, showing that intrinsic structural disorder can be sustained within mammalian cells.
References
- Freedberg DI and Selenko P. Live cell NMR Annu. Rev. Biophys. 2014;43:171–192.
- Sakakibara D, et al. Protein structure determination in living cells by in-cell NMR spectroscopy. Nature 2009;458:102–105.
- Yashroy RC. Magnetic resonance studies of dynamic organisation of lipids in chloroplast membranes. Journal of Biosciences 1990;15(4):281.
- Alderson TA and Bax AD. Parkinson’s Disease. Disorder in the court. Nature 2016; doi:10.1038/nature16871.
- Theillet FX, et al. Structural disorder of monomeric α-synuclein persists in mammalian cells. Nature 2016; doi:10.1038/nature16531.