Advantages and Disadvantages of Novel Oral Anticoagulants (NOACs)
Reporter: Aviva Lev-Ari, PhD, RN
UPDATED ON 2/1/2019
NOACs Usually Preferable to Warfarin in Atrial Fibrillation: Guideline Update
READ ALL GUIDELINES at the sources listed below.
Here we post only,
Triple vs Double Antithrombotic Therapy
The update provides a warning about the extra bleeding risk associated with OAC in patients with AF who have undergone percutaneous coronary intervention (PCI) for ACS, who otherwise would also receive dual antiplatelet therapy (DAPT). Such “triple therapy” is usually best avoided, it emphasizes.
In patients with increased stroke risk (based on a CHA2DS2-VASc ≥2) who’ve had PCI for ACS, the update states, “double therapy” with P2Y12 inhibitor antiplatelets plus a dose-adjusted vitamin-K antagonist, low-dose rivaroxaban, or 150 mg bid dabigatran “is reasonable to reduce the risk of bleeding compared with triple therapy.” The recommendations are IIa, level of evidence B-R.
“The guideline acknowledges that if there’s a need to put them on triple therapy, it should only be for a short period of time: 4 to 6 weeks, for example,” January said. Following that early post-PCI period in which stent thrombosis is most likely, the patient should preferably be transitioned to double therapy.
“DAPT alone may be considered for patients with ACS who have AF and a CHA2DS2-VASc score of 0 to 1, with reconsideration of the indications for anticoagulation over time,” the new document says.
January reported no conflicts. Disclosure information for all writing committee members and reviewers is in the report and tabulated separately online.
- Circulation. Published online January 28, 2019. Report
- J Am Coll Cardiol. Published online January 28, 2019. Report
- Heart Rhythm. Published online January 28, 2019. Report
SOURCE
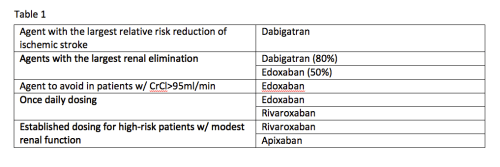
In the past four years, three novel oral anticoagulant (NOAC) medications have become available:
- apixaban (Eliquis®),
- dabigatran (Pradaxa®), and
- rivaroxaban (Xarelto®). A fourth NOAC,
- edoxaban (Savaysa™), has been submitted for approval by the US Food and Drug Administration …
Two small to moderate size trials have shown similar bleeding risk with other NOACs (VENTURE-AF with rivaroxaban [Xarelto] and RE-CIRCUIT with dabigatran [Pradaxa]) compared with vitamin K antagonists. In a non-formal “eyeball” meta-analysis with AXAFA-AFNET 5, combined death, stroke or transient ischemic attack, and major bleeding risk appeared to trend lower with a NOAC than vitamin K antagonist.
However, “differences in populations and procedures may well explain the different outcomes in bleeding rates and silent strokes with NOAC versus vitamin K antagonists,” suggested Blomstrom-Lundqvist.
Increased Bleeding is Main Issue With Newer Agents
Regardless of which agent is used, clinical practice and research has shifted focus to decreasing the risk of bleeding for patients on oral anticoagulants and antithrombotics. While the newer agents might be better than warfarin on several points, the more effective ability to prevent clotting also results in the unwanted consequence of increased bleeding. This sentiment was echoed multiple times by speakers at ACC.16. The most common bleeding complication with NOACs compared to warfarin is gastrointestinal (GI) bleeding. The results of the Ruff meta-analysis favored warfarin over NOACs for rates of GI bleeds (whether results from dabigatran trials were included or not).
“Major bleeds, as well as minor bleeds, may be a problem because patients stop their treatments — not only their antithrombotic treatment, but also the ACE inhibitors, statins and all other life-saving therapies,” explained Freek Verheugt, M.D., FESC, FACC, FAHA, professor of cardiology, Heart-Lung Centre of the University Medical Centre of Nijmegen and chairman of the Department of Cardiology at Onze Lieve Vrouwe Gasthuis, The Netherlands.
Evolution of the Anticoagulant Nomenclature
The approval of dabigatran (Pradaxa) in 2010 lead to the creation of the term new oral anticoagulants (NOACs). This term was changed to novel oral anticoagulants (NOACs) when rivaroxaban (Xarelto) came to the market in 2011. After apixaban (Eliquis) and edoxaban (Savaysa) were cleared, the name changed to direct oral anticoagulants (DOACs) and is the term used by the International Society of Thrombosis and Haemostasis. Alternative names for these agents are target-specific oral anticoagulants (TSOACs) and non-vitamin K oral anticoagulants (NOACs), the term used by the American College of Chest Physicians and the FDA. All of these acronyms refer to the same agents.
Warfarin Use May Not Bring Long-Term Stability for Atrial Fibrillation
Registry study finds INR values fluctuate over 18 months, even in patients considered “stable”